Last week, ProPublica and This American Life published a blockbuster report revealing the inherent risks of acetaminophen, the active ingredient in Tylenol. Each year, acetaminophen overdose sends as many as 78,000 Americans to the emergency room and 150 people die from accidentally overdosing on the pain reliever “hospitals use most.”
As part of our investigation, we created five consumer resources to help you become more aware of acetaminophen toxicity, which the FDA now calls a “persistent, important public health problem.”
1. Drug Lookup

Many common over-the-counter medicines contain acetaminophen, including Theraflu and Nyquil. This tool allows you to easily search for the drugs in your medicine cabinet and see just how much acetaminophen you’re taking.
2. Dose-o-Meter
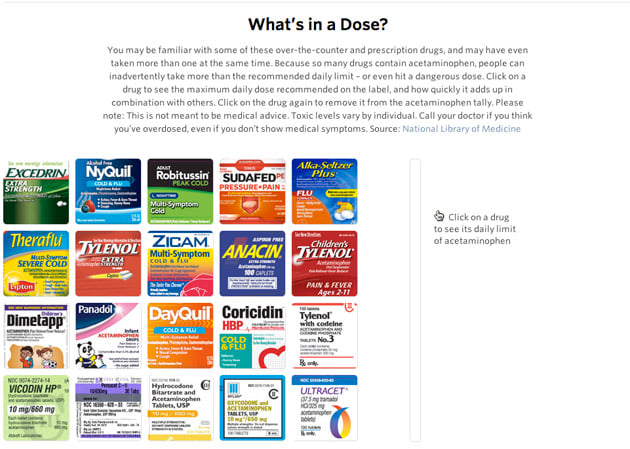
Mixing Tylenol and other medications can quickly put you over the recommended daily dose, and in danger of damaging your liver. Select a group of medicines to see whether you’re still within a safe dosage of acetaminophen.
3. Symptoms of Acetaminophen Poisoning

Overdosing on painkillers can begin with nausea and, in extreme cases, end in death. Use our chart to see the phases of acetaminophen poisoning and its impact on your body.
4. Discussion: Acetaminophen Risks, Safety Measures

Still have questions? Join our live discussion on our investigation this Thursday at 1 pm ET. Our reporter T. Christian Miller will be joined by liver disease specialist Dr. William Lee and pharmaceutical marketing expert PeterMax Miller, to discuss how the FDA and drug company McNeil fought or delayed measures to protect consumers. Weigh in to the chat on our site, or tweet your questions with the hashtag #AcetaChat.
Have you or someone you know suffered from acetaminophen poisoning? Help continue our reporting, and share your story here. And to tell the FDA about your experience, you can fill out a consumer report form.


