Part 1
The Emerald City
Part 2
They're Not Treating Mom Well
Part 3
A Sinking Ship
Part 4
Close the Back Door
Part 1
Life and Death in Assisted Living, Part 1
“The Emerald City”
by A.C. THOMPSON, ProPublica and JONATHAN JONES, special to ProPublica, July 29, 2013

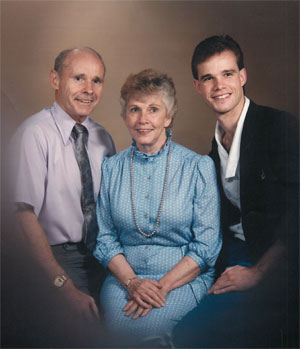
Joan Boice needed help. Lots of it. Her physician had tallied the damage: Alzheimer’s disease, high blood pressure, osteoporosis, pain from a compression fracture of the spine. For Joan, an 81-year-old former schoolteacher, simply getting from her couch to the bathroom required the aid of a walker or wheelchair.
The Alzheimer’s, of course, was the worst. The disease had gradually left Joan unable to dress, eat or bathe without assistance. It had destroyed much of the complex cerebral circuitry necessary for forming words. It was stealing her voice.
Joan’s family was forced to do the kind of hard reckoning that so many American families must do these days. It was clear that Joan could no longer live at home. Her husband, Myron, simply didn’t have the stamina to provide the constant care and supervision she needed. And moving in with any of their three children wasn’t an option.
These were the circumstances that eventually led the Boice family to Emeritus at Emerald Hills, a sprawling, three-story assisted living facility off Highway 49 in Auburn, Calif. The handsome 110-bed complex was painted in shades of deep green and cream, reflecting its location on the western fringe of the craggy, coniferous Sierra Nevada mountain range. It was owned by the Emeritus Corp., a Seattle-based chain that was on its way to becoming the nation’s largest assisted living company, with some 500 facilities stretching across 45 states.
Emeritus at Emerald Hills promised state-of-the art care for Joan’s advancing dementia. Specially trained members of the staff would create an individual plan for Joan based on her life history. They would monitor her health, engage her in an array of physically and mentally stimulating activities, and pass out her 11 prescription medications, which included morphine (for pain) and the anti-psychotic drug Seroquel (given in hopes of curbing some of the symptoms of her Alzheimer’s). She would live in the “memory care” unit, a space designed specifically to keep people with Alzheimer’s and other forms of dementia safe.
At Emerald Hills, the setting was more like an apartment complex than a traditional nursing home. It didn’t feel cold or clinical or sterile. Myron could move in as well, renting his own apartment on the other side of the building; after more than 50 years of marriage, the couple could remain together.
Sure, the place was expensive — the couple would be paying $7,125 per month — but it seemed ideal.
During a tour, a salesperson gave Myron and his two sons, Eric and Mark, a brochure. “Just because she’s confused at times,” the brochure reassured them, “doesn’t mean she has to lose her independence.”
Here are a few things the brochure didn’t mention:
Just months earlier, Emeritus supervisors had audited the facility’s process for handling medications. It had been found wanting in almost every important regard. And, in truth, those “specially trained” staffers hadn’t actually been trained to care for people with Alzheimer’s and other forms of dementia, a violation of California law.
The facility relied on a single nurse to track the health of its scores of residents, and the few licensed medical professionals who worked there tended not to last long. During the three years prior to Joan’s arrival, Emerald Hills had cycled through three nurses and was now employing its fourth. At least one of those nurses was alarmed by what she saw, telling top Emeritus executives — in writing — that Emerald Hills suffered from “a huge shortage of staff” and was mired in “total dysfunction.”

During some stretches, the facility went months without a full-time nurse on the payroll.
The paucity of workers led to neglect, according to a nurse who oversaw the facility before resigning in disgust. Calls for help went unanswered. Residents suffering from incontinence were left soaking in their own urine. One woman, addled by dementia, was allowed to urinate in the same spot in the hallway of the memory care wing over and over and over.
The brochure also made no mention of the company’s problems at its other facilities. State inspectors for years had cited Emeritus facilities across California, faulting them for failing to employ enough staff members or adequately train them, as well as for other basic shortcomings.
Emeritus officials have described any shortcomings as isolated, and insist that any problems that arise are promptly addressed. They cite the company’s growing popularity as evidence of consumer satisfaction. They say that 90 percent of people who take up residence in assisted living facilities across the country report being pleased with the experience.
Certainly, the Boice family, unaware of the true troubles at Emerald Hills, was set to be reassured.
“We were all impressed,” recalled Eric Boice, Joan’s son. “The first impression we had was very positive.”
And so on Sept. 12, 2008, Joan Boice moved into Room 101 at Emerald Hills. She would be sharing the room with another elderly woman. After a succession of tough years, it was a day of great optimism.
Measuring the dimensions of his mother’s new apartment, Eric Boice sought to recreate the feel of her bedroom back home. He arranged the furniture just as it had been. He hung her favorite pictures in the same spots on the wall. On her dresser, he set out her mirror and jewelry box and hairbrush.
Joan, 5-foot-2 and shrinking, had short snow-and-steel hair and wintry gray-blue eyes. Eric looked into those eyes that day at Emerald Hills. He thinks he might have seen a flicker of fear. Or maybe it was just confusion, his mom still uncertain where, exactly, she was.
A Reform Movement Winds Up on Wall Street
The Emeritus Corp., the assisted living corporation now entrusted with Joan’s life, sat atop an exploding industry.
Two decades earlier, Keren Brown Wilson had opened the nation’s first licensed assisted living facility in Canby, Ore., a small town outside of Portland. Wilson was inspired by tragedy: A massive stroke had paralyzed her mother at the age of 55, forcing her into a nursing home, where she was miserable, spending the bulk of her days confined to a hospital bed.
Wilson aimed to create an alternative to nursing homes. She envisioned comfortable, apartment building-style facilities that would allow sick and fragile seniors to maintain as much personal autonomy as possible.
“I wanted a place where people could lock the door,” Wilson explained. “I wanted a place where they could bring their belongings. I wanted a place where they could go to bed when they wanted to. I wanted a place where they could eat what they wanted.”

These “assisted living” facilities would offer housing, meals and care to people who could no longer live on their own but didn’t need intensive, around-the-clock medical attention. The people living in these places would be called “residents” — not patients.
It took Wilson nine years to persuade Oregon legislators to rewrite the state’s laws, a crucial step toward establishing this new type of facility. After that, states across the country began adopting the “Oregon model.”
But what began as a reform movement quickly morphed into a lucrative industry. One of the early entrants was Emeritus, which got into the assisted living business in 1993, opening a single facility in Renton, Wash. The company’s leader, Daniel Baty, had his eyes on something much grander: He was, he declared, aiming to create a nationwide chain of assisted living facilities.
Two years later, Baty took the corporation public, selling shares of Emeritus on the American Stock Exchange, and piling up the cash necessary to vastly enlarge the company’s footprint. Many of Emeritus’s competitors followed the same path.
The company’s rapid growth was, at least in part, a reflection of two significant developments. Americans were living longer, with the number of those in the 65-plus age bracket ballooning further every year. And this growing population of older Americans was willing to spend serious money, often willing to drain their bank accounts completely to preserve some semblance of independence and dignity — in short, something of their former lives.
As the assisted living business flourished, the federal government, which oversees nursing homes, left the regulation of the new industry to the states, which were often unprepared for this torrent of expansion and development. Many states didn’t develop comprehensive regulations for assisted living, choosing instead to simply tweak existing laws governing boarding homes.
In this suddenly booming, but haphazardly regulated industry, no company expanded more aggressively than Emeritus. By 2006, it was operating more than 200 facilities in 35 states. The corporation’s strategy included buying up smaller chains, many of them distressed and financially troubled, with plans to turn them around.
Wall Street liked the model. Market analysts touted the virtues of the company and its stock price floated skyward. One of the corporation’s appeals was that its revenues flowed largely from private bank accounts; unlike hospitals or nursing homes, Emeritus wasn’t reliant on payments from the government insurance programs Medicare or Medicaid, whose reimbursement rates can be capped. As the company noted in its 2006 annual report, nearly 90 percent of its revenues came from “private pay residents.”
In filings with the Securities and Exchange Commission and in conference calls with investors, Emeritus highlighted many things: occupancy rates; increasing revenue; a constant stream of complex real estate deals and acquisitions; the favorable demographic trends of an aging America.
“The target market for our services is generally persons 75 years and older who represent the fastest growing segments of the U.S. population,” Emeritus stated in a 2007 report filed with the SEC.
Today, the assisted living industry rivals the scale of the nursing home business, housing nearly three-quarters of a million people in more than 31,000 assisted living facilities, according to the U.S. Department of Health and Human Services.
Keren Brown Wilson, the early and earnest pioneer of assisted living, is happy that ailing seniors across the country now have the chance to spend their final years in assisted living facilities, rather than nursing homes. But in her view, the rise of assisted living corporations — with their pursuit of investment capital and their need to please shareholders — swept in “a whole new wave of people” more focused on “deals and mergers and acquisitions” than caring for the elderly.
She speaks from experience. After her modest start, Wilson went on to lead a company called Assisted Living Concepts, and took it onto the stock market. Wilson left the company in 2001, and it has encountered a raft of regulatory and financial problems over the last decade.
“I still have a lot of fervor,” said Wilson, who now runs a nonprofit foundation and teaches at Portland State University. “I believe passionately in what assisted living can do. And I’ve seen what it can do. But for some of the people, it’s just another job, or another business. It’s not a passion.”
“A Phenomenal Deal”

Joan Boice, born Joan Elizabeth Wayne, grew up in Monmouth, Ill. It was a tiny farm belt community, not far from the Iowa border. Her father, a fixture in the local agriculture trade, owned a trio of riverfront grain elevators on the Mississippi and a fleet of barges. As a teenager, she spent her summers trudging through the fields, de-tasseling corn.
In 1952, accompanied by a friend, Joan packed up a car and followed the highway as far west as it would go. Then in her early 20s, she was propelled by little more than the notion that a different life awaited her in California. In a black-and-white snapshot taken shortly after she arrived, Joan is smiling, a luxuriant sweep of dark hair framing her pale face, gray waves curling in the background. It was the first time she’d seen the Pacific.
Joan had been a teacher for two years in Illinois, and she quickly found a job at an elementary school in Hayward, a suburb of San Francisco. In certain regards, her outlook presaged the progressive social movements that were to remake the country during the next two decades. She viewed education as a “great equalizing force” that could help to remake a society far too stratified by class, race and gender.
“She was just free-spirited and confident,” Eric, her son, said.
Joan met Myron Boice through a singles group at a Presbyterian church in Berkeley. On their wedding day, Joan flouted convention by showing up in a blue dress. The Boice children came along fairly quickly: Nancee, then Mark, then Eric.
Myron Boice was a dreamer. A chronic entrepreneur. He sold tools from a van. He made plans to open restaurants. He had one idea after another. Some worked; others didn’t.
Joan’s passion for education never dissipated. Even in her late 60s, she continued to work as a substitute teacher in public schools. After retirement, she began volunteering with a childhood literacy program.
But age eventually tightened its grip, and hints of a mental decline began surfacing around 2005. Eric grew worried when she couldn’t figure out how to turn on her computer twice in the span of a few months. Then she forgot to include a key ingredient while baking a batch of Christmas cookies. The cookies were inedible.
The elderly couple was still living in the San Francisco suburbs, when, in late 2006, a doctor diagnosed Joan with Alzheimer’s. As her mind deteriorated, Myron struggled to meet her needs. The situation was worsened by the fact that none of the children lived nearby. Mark was in Ohio. Nancee was about an hour away in Santa Cruz. And Eric and his wife, Kathleen, were roughly two hours away in the foothills of the Sierra.
“We offered my parents to come and live with us,” Eric recalled. But Myron said no. He and Joan wouldn’t move in with any of the kids. The family patriarch refused to become a burden.
A physician encouraged Joan and Myron to consider assisted living. It made sense. And so Myron sold their home in 2007 and the couple moved into a facility called The Palms, near Sacramento. The move put them approximately 40 minutes away from Eric and Kathleen.
“They were very attentive to every single thing she needed,” Kathleen Boice said of the staff at The Palms. “They actually re-taught her to eat with a fork and a knife.”
By 2008, however, Myron wanted a change. He wanted to be closer to his son and daughter-in-law and grandkids. He wanted different meals, a new environment. Myron began hunting for a new place to live, a search that led to Emeritus at Emerald Hills in Auburn.
Emeritus opened the Emerald Hills complex in 1998. It was, in many ways, a classic Emeritus facility, situated in a middle-class locale that was neither impoverished nor especially affluent. It was a sizable property, capable of housing more than 100 people.
In part because of its appetite for expansion, Emeritus was in the early stages of what proved to be a period of enormous stress. In 2007, the company had made its biggest acquisition to date, buying Summerville Senior Living Inc., a California-based chain with 81 facilities scattered across 13 states.
The purchase — which expanded Emeritus’s size by roughly one-third — helped the company make another major leap, bouncing from the low-profile American Stock Exchange into the big leagues of commerce, the New York Stock Exchange. News of the Summerville deal propelled the company’s stock to a new high. Emeritus was poised to become the nation’s No. 1 assisted living chain.

But the timing for this bold move turned out to be wretched. The real estate market was freezing up, and it would soon collapse, plunging the nation into an epochal recession. For Emeritus, the economic slowdown and then the housing crash posed direct challenges. Its services didn’t come cheap, so many people needed to sell their homes before they could afford to move into the company’s facilities. With the real estate market calcified, Emeritus’s customer pool shrank.
“Our stock price plummeted,” recalled Granger Cobb, Emeritus’s chief executive officer, who joined the company as part of the Summerville deal. The company’s occupancy rates had been trending skywards. Now they went flat.
At Emerald Hills, the economic slowdown that summer was making life tough for Melissa Gratiot, the lead sales agent.
“It was way harder to move residents in,” she remembered.
But there was some good news. She was close to a significant sale, this one to a couple. Gratiot worked the pitch. She talked with the family. She emailed. She gave them a tour of the facility’s memory care unit, called The Emerald City. She told the family she’d received approval from higher ups to offer the family “a phenomenal deal.”
Gratiot closed the sale. On Aug. 29, 2008, Myron and Eric signed the contract, and the family opened its wallet: A $2,500 initial move-in fee; $2,772 for Joan's first two weeks in Room 101; another $1,660 for Myron.
There had been one oversight, though. No one at Emeritus with any medical training had ever even met Joan, much less determined whether Emerald Hills could safely care for her.
Correction (7/29): An earlier version of this story stated that Emeritus at Emerald Hills had failed a company audit of its memory care unit before Joan Boice moved in. It has been corrected to say an audit found flaws in the facility’s medication handling process before Boice moved in. The memory care unit was audited while Boice was living there and failed nearly every important test.
Life and Death in Assisted Living, Part 2
“They’re Not Treating Mom Well”

When the ambulance crew arrived, about 8:20 p.m., Joan Boice was in the TV lounge, face-down on the carpet. Her head had struck the floor with some velocity; bruises were forming on her forehead and both cheeks. It appeared she’d lost her balance and fallen out of a chair.
But no one at the assisted living facility could say precisely how the accident had occurred. No one knew how long Joan had been splayed out on the floor. She had defecated and urinated on herself.
Worried that Joan might have injured her spine, the emergency medical personnel gently rolled her over and placed her on a back board. They pumped oxygen into her nostrils.
It was Sept. 22, 2008 — just 10 days after Joan had first moved into Emerald Hills.
No Emeritus employees accompanied Joan to the hospital. And even though Joan’s husband, Myron, was living in the facility, the Emeritus workers didn’t immediately alert him that Joan had fallen and hurt herself. Joan, confused, injured, and nearly mute, ended up in the local hospital by herself, surrounded by strangers.
It was supposed to have been a festive night for Joan’s son Eric and his wife, Kathleen, who lived nearby. They were throwing a birthday party for their daughter, then in elementary school. The celebration was interrupted when a doctor called from the hospital with news of Joan’s fall. As Kathleen recalled it, the physician was somewhat baffled — he didn’t understand what Joan was doing in the emergency room without a family member, and he was having trouble deducing the extent of her injuries because she couldn’t communicate.
California law requires assisted living companies to conduct a “pre-admission appraisal” of prospective residents, to ensure they are appropriate candidates for assisted living.
But Emerald Hills took Joan in without performing an appraisal. It wasn’t for lack of time. The Boices had signed the contract to live at Emerald Hills more than two weeks before Joan moved in.
Joan, then, had taken up residence in the memory care unit at Emerald Hills. The unit — referred to as a “neighborhood” by the company — is a collection of about a dozen small apartments on either side of a central hallway. At each end of the hallway are heavy doors equipped with alarms, which sound when anyone enters or leaves. The alarm system is meant to prevent residents from simply walking off.
On the day Joan moved into Room 101 in the unit, a company nurse named Margaret “Peggy” Stevenson briefly looked her over. The nurse realized that Joan needed to be monitored closely to keep her from falling — she wrote it down in her cursory assessment — but facility records show she didn’t craft any kind of detailed plan for her care and supervision.
Stevenson, asked years later about Joan, said she could recall nothing about her or her stay at Emerald Hills.
Kathleen had immediate suspicions about Joan’s fall. The family, she said, had warned the facility not to leave Joan sitting in a chair without supervision because she was liable to try to stand up, lose her balance, and topple to the floor. Joan had fallen several times during an earlier stay in an assisted living facility near Sacramento, but the staff had developed a specific plan to address the issue.
Despite the warning, Kathleen said that when she visited Emerald Hills during Joan’s first days there she often found her mother-in-law sitting in a chair alone.
The recent track record at Emerald Hills featured a host of falls similar to Joan’s, and ambulances were often called to take the injured off to the hospital. Falls are a particular hazard for the elderly, and assisted living facilities like Emerald Hills are required to report them to state regulators.
Internal company records documented 112 falls at Emerald Hills in 2008. Some residents fell repeatedly.
Consider the case of one Emerald Hills resident, 83-year-old Dorothy “Dottie” Bullock.
On April 5, 2008, an Emeritus employee discovered Bullock “on the floor in a semi-seated position” in the memory care unit, according to a state report. She “was unable to tell” the worker what had happened to her. The incident was described as a fall in state records. Emerald Hills sent her to the hospital.
On April 7, Bullock, back at Emerald Hills, fell again, according to the handwritten log of her personal attendant, who was hired by Bullock’s husband to give her extra help.
On April 8, Bullock, complaining of pain, was hauled by ambulance back to the hospital. Doctors concluded that she’d fractured her pelvis, but soon returned her to Emerald Hills. She fell again on April 12.
Bullock would fall again months later, for the final time.

Emeritus records show Bullock tumbled in front of her apartment and was found on the carpet with her aluminum walker beneath her. Blood spilled from her nose and a “bump” developed on her forehead, according to the company documents. The impact broke a vertebra in Bullock’s neck and crushed her nasal bones and sinus structures, hospital records show. A CT scan revealed possible fractures of both eye-sockets and the base of the skull.
Dottie Bullock died in the emergency room.
While Emeritus recorded the fatality in its internal logs, the company did not report her death to state regulators, a violation of California law. The state requires assisted living facilities to file reports on all deaths, even those believed to be from natural causes, so that it can look into suspicious or troubling incidents.
Emeritus said it lacked information about Bullock’s death and thus could not say why it had occurred.
Bullock’s personal attendant, Julie Covich, says Bullock was not supervised properly.
“I think there was neglect,” said Covich, who usually visited Emerald Hills once or twice a week to help out Bullock. “I would go in there and never see a caregiver.”
“It was hard to find anyone that was running the place,” she said. “It was crazy.”
“Heads on the Beds”
In early 2008, the year Joan Boice entered Emerald Hills, Emeritus rolled out a new business campaign. The company dubbed it the “No Barriers to Sales” effort.
The concept was straightforward: Move as many people as possible into Emeritus facilities. Wall Street was looking closely at the company’s quarterly occupancy numbers and a few percentage points could propel the stock price upward or send it tumbling down.
With the housing market foundering, Emeritus needed to step up its sales efforts.
In case there was any confusion about just how seriously the company took this new campaign, a company vice president sent a blast email to facility directors across California. In the body of the email, the vice president got right to it: “SALES and your commitment to sales is your highest priority right now.” Facility directors, the message concluded, would be “held responsible for census and occupancy growth.”
Emeritus employees across the country realized they were entering a new era.
“There was a different sense of urgency. The tone was different,” said a former Emeritus manager who ran a facility at the time. “The message from above was put as many people as possible in the beds and make as much money as possible. That’s what they said. Verbatim. Honestly.”
According to Lisa Paglia, a regional executive in California at the time, Budgie Amparo, the company’s top official for quality control, was openly critical when a Northern California facility declined to admit someone who did not have a doctor’s evaluation.
Such evaluations, which are designed to keep out seniors with problems that assisted living facilities aren’t equipped to handle, are required under a California law known as Title 22.
But on a conference call with roughly half a dozen California managers, Paglia said, Amparo declared that the Northern California facility should have admitted the resident.
“Our priority,” Amparo declared, according to Paglia, “is to get the heads on the beds.”
The issue arose again in October 2008 during a training session for approximately 25 facility directors and salespeople held at an Emeritus property in Tracy, Calif. During the seminar, a company vice president reiterated Amparo’s instruction to disregard California law, according to court records and interviews.
The mandate prompted something of a staff revolt.
At least one facility director spoke out at the meeting: His license to operate the facility was at stake, he said.
An employee who worked at the Tracy facility eventually alerted California regulators. The state dispatched an investigator, and state records show that the investigator met with employees who confirmed that a company official had approved the practice of admitting someone without a doctor’s report. The investigator reviewed a random sample of seven resident files, finding that two people had been moved in illegally, documents show.
Amparo, a nurse whose full title is executive vice president of quality and risk management, denies directing employees to violate the regulation. In a written statement, Emeritus said, “Neither Budgie Amparo nor any of our other officers issued a directive to violate Title 22 or any other law. Emeritus does not condone allowing residents to move in without the proper documents.”
Emeritus eventually fired Paglia, and lawyers for the company have since portrayed her as a poor worker who failed to do her job competently. Along with two other former Emeritus employees, Paglia sued the company alleging wrongful termination, and wound up settling on secret terms.
For assisted living chains such as Emeritus, there is a powerful business incentive to boost occupancy rates and to take in sicker residents, who can be charged more.
Emeritus, for its part, rejects any suggestion that a quest for profits has tainted its admission practices. But in interviews, former Emeritus executives described a corporate culture that often emphasized cash flow above all else. The accounts of the executives, who spoke independently but anonymously, were strikingly consistent.
“It was completely focused on numbers and not human lives,” said one executive, who worked for Emeritus for more than three years and oversaw dozens of facilities in Eastern states.
The company’s emphasis on sales and occupancy rates, the executive said, transformed the workforce into “a group of people who were grasping at every single lever they could pull to drive profitability.”
Emeritus operates a sophisticated, data-driven sales machine. There are occupancy goals for each facility, as well as yearly company-wide goals. The company tracks dozens of data points — including every move-in and move-out of residents — in a vast database. It posts a monthly snapshot of each facility’s sales statistics on an internal website, allowing employees to see which strategies are most successful.
Sales specialists are instructed on how to use psychology to persuade potential customers to sign on. One suggestion: Give the customer “a sense of control and choice by offering two possible options.” A 2009 Emeritus sales manual, which runs 181 pages, encourages sales people to generate publicity by hosting seminars on Alzheimer’s or organizing charity efforts in the event of a natural disaster like a “flood or earthquake.”
Emeritus motivates its workforce with a broad range of financial incentives. There are bonuses for hitting monthly occupancy goals. Bonuses for hitting yearly occupancy goals. Bonuses for boosting overall earnings. And the money doesn’t just go to sales people: The company hands out checks to maintenance workers, nurses, facility directors and other workers.
Nurses play a key role in assisted living, providing much of the hands-on care. But nurses at Emeritus facilities are also expected to be deeply involved in increasing revenue by making sales.
During more than a year of reporting, ProPublica and PBS Frontline spoke to 10 facility directors who said nurses were required to participate in weekly conference calls focusing on little but economics. Those accounts are backed by an internal Emeritus document that lays out the agenda for the weekly calls and that shows an overarching concentration on finances.
Doris Marshall was at the forefront of Emeritus’s efforts to have nurses play the dual roles of caregivers and salespeople. After receiving her nursing license in 1984, Marshall had spent many years tending to patients in the emergency department of a Southern California hospital, and she’d later gone on to help run a nursing school.
But Marshall was intrigued by the assisted living business and in March 2008 she signed on to supervise 10 Emeritus properties scattered across Northern California. Amparo, the company’s head nurse, convinced Marshall to take the job, telling her nurses “had a voice” at Emeritus.
Marshall was to oversee the well-being of roughly 800 elderly people. But her job description went well beyond that: She was to help with “marketing” and “attaining financial goals.” Her job, in the end, actually involved very little nursing.
Instead, she said, she was drawn into Emeritus’s evolving strategies aimed at upping its revenues. The company planned to bring in more seniors with Alzheimer’s and dementia because they could be charged more, she said. Her boss gave her a digital tracking tool showing how much more money Emeritus could make by admitting sicker, frailer residents.
By the fall of 2010 Marshall was worn out and disillusioned. She quit.
Emeritus’s extraordinary drive to put heads in beds — perhaps routine in, say, the hotel industry — has distorted the admissions process at some facilities, records and interviews show. Since 2007, state investigators have cited the company’s facilities more than 30 timesfor housing people who should have been prohibited from dwelling in assisted living facilities.
A 2010 episode at an Emeritus facility in Napa highlighted the perils of improperly admitting people. The facility rented a room to a 57-year-old woman with an eating disorder, depression, bipolar disorder and a history of suicide attempts. The woman, who was distraught over the death of her husband, taped a note to her door saying she wasn’t to be disturbed and committed suicide, overdosing on an amalgam of prescription painkillers.
The state’s investigation into the death was scathing: the woman should never have been allowed to move in; the staff had missed or ignored bulimic episodes and her obvious weight loss; no plan of care was ever developed or implemented despite the resident’s profound psychological problems.
Emeritus, asked to respond to the state’s investigation, said only that the woman had overdosed on drugs she had brought into the facility on her own, and that as a result they could not be faulted in her death.
“She Barely Even Talked to Us”

In the aftermath of her fall in September 2008, Joan returned to Emerald Hills. But the staff, inexperienced and often exhausted, worried about her.
“She couldn’t walk, she couldn’t feed herself, she barely even talked to us, and her health wasn’t that good,” recalled Jenny Hitt, a former medication technician at Emerald Hills.
But if concern was abundant at Emerald Hills, expertise was in short supply.
Alicia Parga ran Joan’s memory care unit. On some weekends, she managed the entire building — not only the wing of residents with dementia, but the rest of the three-story assisted living facility, one that could hold a total of more than 100 residents.
After Parga started on the job, it took Emeritus roughly 18 months to give her any training on Alzheimer’s and dementia. The state regulations were hardly substantial: Someone such as Parga was obligated to get six hours of training during her first four weeks on the job. But even that requirement wasn’t met.
Emeritus has insisted that Emerald Hills had properly trained personnel to care for Joan and others, and they described Parga as a woman deeply invested in tending to the residents.
But Parga, who had barely earned a high school degree, wasn’t even familiar with the seven stages of dementia. Though she was responsible for the well-being of 15 or more seriously impaired people, as well as the supervision of employees, Parga was paid less than $30,000 per year.
Catherine Hawes, a health care researcher at Texas A&M University, conducted the first national study of assisted living facilities. In her view, training is absolutely crucial. A well-educated employee can “interpret non-verbal cues” from people like Joan, intercept seniors before they wander away from the building, or keep residents from eating or drinking poisonous substances.
“You can do great care,” she said. “You just — you’ve got to know how.”
Other than the Emeritus employees working in the memory care unit at Emerald Hills, only one person saw Joan enough to know what kind of daily care she was getting: Her husband, Myron.
He was worried. And he did his best to sum up his concerns to his son Eric:
“They’re not treating Mom well.”
Life and Death in Assisted Living, Part 3
“A Sinking Ship”

On Sept. 30, 2008, an employee at the Emerald Hills assisted living facility in Auburn, Calif., made an entry in a company computer log: “pressure ulcer/wound.”
Joan, who had spent just 19 days in the facility, had developed the wound on her foot. The fall eight days earlier had hospitalized her and left her with bruises and an abrasion on her right temple. This, though, could be much, much worse.
Pressure ulcers — also known as bed sores — can form when a person loses the ability to move about freely. Lying in bed or sitting in a chair for long stretches of time diminishes the blood flow to the skin, causing it to break down and die. A hole grows. If bacteria creep into the wound, the bugs can devour flesh or invade the blood and bones. Pressure ulcers can turn fatal, particularly in older people.
Because of the lethal potential of pressure ulcers, the federal government monitors them closely in the nursing home business. In the eyes of experts, the sores are often an indicator of poor care. Attentive caregivers can prevent many pressure sores by making sure that people don’t spend too much time in the same position.
“We know that most bed sores are avoidable,” said Kathryn Locatell, a forensic geriatrician who investigates allegations of elder abuse for California Department of Justice. “That is the consensus of experts in the field.”
Physicians grade the ulcers on a scale ranging from Stage 1 to Stage 4, with Stage 4 being the most serious. In California, assisted living facilities are allowed to house people with Stage 1 and 2 sores, but only if the resident receives medical treatment from a “skilled professional.” The law bars facilities from renting rooms to people with more severe pressure ulcers.
The Emerald Hills worker who wrote up Joan’s pressure ulcer on Sept. 30 understood its significance. The employee noted that a “skilled professional” would be treating the wound.
Emerald Hills was supposed to contact Joan’s doctor when she developed the ulcer. But nobody from Emerald Hills called a doctor. No nurse came to salve Joan’s wound. And nobody told Joan’s relatives — her husband, Myron, who lived in the same facility, or her son who lived nearby — about the development.
Joan’s short, painful stay at Emerald Hills seemed to be accelerating her decline.
Things had been different at the first assisted living facility Joan had lived at, a place called The Palms near Sacramento. There she’d enjoyed a constant stream of activities. “She was doing things every day,” remembered Eric Boice, her son. There were storytelling sessions, games of wheelchair bowling, arts and crafts. Once Joan had smeared finger paint on her palm and pressed it to a piece of paper, creating a keepsake for her son.
Adequate staff at The Palms was central to the family’s satisfaction with Joan’s stay. Promises that staff would keep Joan active and engaged — central ambitions in dementia care — were kept. And the perils of prolonged inactivity, like mental decline and dangerous sores, were avoided.
By comparison, the unit at Emerald Hills where Joan lived seemed to the family to be poorly staffed and thus static. Staff rarely turned up to organize activities. What few staffers were available managed only to bring Joan down to the TV lounge, where she sat, unengaged. Myron and other family members visited frequently, but otherwise she was marooned.
Melissa Gratiot, the Emeritus salesperson who had convinced the Boices to come to Emerald Hills, had given the family a brochure during her sales pitch. The facility’s “entire staff” would strive to produce “meaningful interactions and activities” for Joan.
But Gratiot had come to doubt her own marketing pitch, and a lack of staff was p
Follow ProPublica
Most Read
Republish This Story for Free
Creative Commons License (CC BY-NC-ND 3.0)
Thank you for your interest in republishing this story. You are are free to republish it so long as you do the following:
- You have to credit ProPublica and any co-reporting partners. In the byline, we prefer “Author Name, Publication(s).” At the top of the text of your story, include a line that reads: “This story was originally published by ProPublica.” You must link the word “ProPublica” to the original URL of the story.
- If you’re republishing online, you must link to the URL of this story on propublica.org, include all of the links from our story, including our newsletter sign up language and link, and use our PixelPing tag.
- If you use canonical metadata, please use the ProPublica URL. For more information about canonical metadata, refer to this Google SEO link.
- You can’t edit our material, except to reflect relative changes in time, location and editorial style. (For example, “yesterday” can be changed to “last week,” and “Portland, Ore.” to “Portland” or “here.”)
- You cannot republish our photographs or illustrations without specific permission. Please contact [email protected].
- It’s okay to put our stories on pages with ads, but not ads specifically sold against our stories. You can’t state or imply that donations to your organization support ProPublica’s work.
- You can’t sell our material separately or syndicate it. This includes publishing or syndicating our work on platforms or apps such as Apple News, Google News, etc.
- You can’t republish our material wholesale, or automatically; you need to select stories to be republished individually. (To inquire about syndication or licensing opportunities, contact [email protected].)
- You can’t use our work to populate a website designed to improve rankings on search engines or solely to gain revenue from network-based advertisements.
- We do not generally permit translation of our stories into another language.
- Any website our stories appear on must include a prominent and effective way to contact you.
- If you share republished stories on social media, we’d appreciate being tagged in your posts. We have official accounts for ProPublica on Twitter, Facebook and Instagram.
Copy and paste the following into your page to republish:





