When Renee
Royak-Schaler unexpectedly collapsed and died on May 22, no one ordered an
autopsy.
Not the
doctors at Howard County General Hospital in Columbia, Md., where the
64-year-old professor and cancer researcher was pronounced dead.
Not the
Maryland Office of the Chief Medical Examiner, which passed on the case because
no foul play was involved.
And not
Royak-Schaler’s physicians at Johns Hopkins University School of Medicine who
had diagnosed cancer in her hip two days beforehand but acknowledged they
didn’t know what had caused her unforeseen death.
A half-century ago, an autopsy would have been
routine. Autopsies, sometimes called the ultimate medical audit, were an
integral part of American health care, performed on roughly half of all
patients who died in hospitals. Today, data from the Centers for Disease
Control and Prevention show, they are conducted on about 5 percent of such
patients.

Dr. Jeffrey Schaler addresses family and friends gathered to remember his late wife, Dr. Renee Royak-Schaler. (Jenna Isaacson Pfueller/ ProPublica)
As Royak-Schaler’s husband, Jeffrey Schaler,
discovered, even sudden unexpected deaths do not trigger postmortem reviews.
Hospitals are not required to offer or perform autopsies. Insurers don’t pay
for them. Some facilities and doctors shy away from them, fearing they may
reveal malpractice. The downward trend is well-known — it’s been studied
for years.
What has not been
appreciated, pathologists and public health officials say, are the far-reaching
consequences for U.S. health care of minuscule autopsy rates.
Diagnostic errors,
which studies show are common, go undiscovered, allowing physicians to practice
on other patients with a false sense of security. Opportunities are lost to
learn about the effectiveness of medical treatments and the progression of
diseases. Inaccurate information winds up on death certificates, undermining the
reliability of crucial health statistics.
It was only
because of Royak-Schaler’s connections that her case ended differently. Her
colleagues at the University of Maryland School of Medicine urged her husband
to authorize an autopsy and volunteered to conduct it for free.

Friends and family of Dr. Renee Royak-Schaler attend a memorial service in her honor at Westminster Hall on the University of Maryland School of Medicine campus where she worked. (Jenna Isaacson Pfueller/ ProPublica)
In her case,
as in so many, the autopsy revealed a surprise: Royak-Schaler, the renowned
cancer researcher, had cancer ravaging her body — in her lungs, kidneys,
abdomen and the marrow of her bones. A blood clot, likely related to the
tumors, caused her sudden death.
Jeffrey
Schaler has wrestled with anger that his wife wasn’t diagnosed sooner but said
knowing how she died was better than not.
“There’s a
sense of peace that accompanies that knowledge,” he said.
For
the last year, ProPublica, PBS “Frontline” and NPR have probed America’s deeply flawed system of death investigation, focusing primarily
on forensic autopsies, which are conducted by coroners’ offices and medical
examiners when there is suspicion of an unnatural death. State laws vary, but the
preponderance of deaths that occur in hospitals are considered natural. When
deaths are unexplained, unobserved or within 24 hours of admission, hospitals
may be required to report them to local coroners or medical examiners, but such agencies rarely take hospital cases.
Hospital physicians,
with consent from patients’ next of kin, may order a clinical autopsy to
explore the disease process in the body and determine the cause of death. That
was the norm 50 years ago, when the value of the autopsy was considered
self-evident.
“Much of what we know
about medicine comes from the autopsy,” said Dr. Stephen Cina, chairman of the forensic
pathology committee for the College of American Pathologists. “You really can’t say for sure what went on or
didn’t go on without the autopsy as a quality assurance tool.”
Yet, autopsy
rates at teaching hospitals, which are typically run on a nonprofit basis and
have an educational mission, hover around 20 percent today. At private and
community hospitals, which constitute 80 percent of facilities nationwide,
rates can be close to zero.
“I know new
hospitals are being built these days without a place to do an autopsy,” said
Dr. Dean Havlik, the Mesa County, Colo., coroner, who estimated that the
overall hospital autopsy rate in his area is less than 1 percent.
Hospitals
have powerful financial incentives to avoid autopsies. An autopsy costs about
$1,275, according to a survey of hospitals in eight states. But Medicare and
private insurers don’t pay for them directly, typically limiting reimbursement
to procedures used to diagnose and treat the living. Medicare bundles payments for autopsies into overall payments to
hospitals for quality assurance, increasing the incentive to skip them, said
Dr. John Sinard, director of autopsy service for the Yale University School of
Medicine.
“The hospital is going to get the money whether
they do the autopsy or not, so the autopsy just becomes an expense,” Sinard
said.
Since a 1971
decision by The Joint Commission, which accredits health-care facilities,
hospitals haven’t had to conduct autopsies to remain in good standing. The
commission had mandated autopsy rates of 20 percent for community hospitals and
25 percent for teaching facilities, but dropped the requirement. Many hospitals
were performing autopsies “simply to meet the numbers” and not to improve
quality, said Dr. Paul Schyve, the commission’s senior adviser of health-care
improvement.
Doctors,
too, have gravitated away from autopsies because of growing confidence in
modern diagnostic tools such as CT scans and MRIs, which can identify ailments
while patients are still alive.
Still, in
study after study, autopsies have revealed that doctors make a high rate of
diagnostic errors even with increasingly sophisticated imaging equipment.
A 2002
review of academic studies by the federal Agency for Healthcare Research and
Quality found that when patients were autopsied, major errors related to the
principle diagnosis or underlying cause of death were found in one of four
cases. In one of 10 cases, the error appeared severe enough to have led to the
patient’s death.
“Clinicians
have compelling reasons to request autopsies far more often than currently
occurs,” the agency concluded.
Schyve
called the findings of such studies flawed because cases in which autopsies are
performed are typically the most complex, making diagnostic errors more likely.
The overall error rate is far lower, he said.
But Sinard
said so few autopsies are being conducted — one survey found that 63
percent of hospitals in Louisiana performed none in a given year — that
doctors and hospitals can’t say for certain how patients are dying. “They’ve
never checked,” the Yale pathologist said.
Pathologists
interviewed by ProPublica said they often find diagnostic errors. “We often identify things that the imaging study could not,” said Dr.
Debra Kearney, director of autopsy pathology at Texas Children’s Hospital.
Autopsies
can also be a crucial tool for evaluating and improving medical care.
Dr. Elizabeth Burton, deputy director of the pathology department at Johns Hopkins University
School of Medicine, said performing autopsies on patients who have
died of hospital-acquired infections helps save others. Infection clusters “go in waves” in
hospitals, she said. Physicians have used her findings to change antibiotic
regimens, snuffing out the bacterium.
Dr. Renu
Virmani, president and medical director of the nonprofit CVPath Institute, has
used postmortem examinations to help reform the treatment of heart disease.
Virmani and her team have collected about 250 specimens of metal stents removed
at autopsy from patients who had procedures to clear blockages from their
arteries.
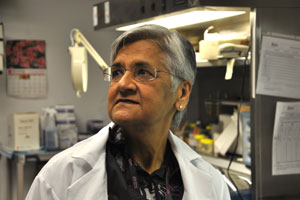
Dr. Renu Virmani, a pathologist, in her lab in Gaithersburg, Maryland. With the use of autopsies, her research helped change the way patients with certain heart conditions are treated in America. Dr. Virmani says she finds the low rates of autopsies done on patients who die in a hospital to be alarming. (Habiba Nosheen/ProPublica)
Their work
showed that, in certain patients, a type of stent designed to reduce the risk
of blood clots was causing delayed healing, inflammation and reactions that
could be fatal. As a result, patients who receive these stents are now required
to take blood-thinning medication for a year after the procedure.
Sitting in
her lab in Gaithersburg, Md., Virmani peers through a microscope at a specimen
slide taken from a 61-year-old man who died suddenly in 2004, about four months
after receiving a clot-resistant stent. She points out signs of inflammation in
the cross-section of his stented artery, describing the swirls and grains,
stained pink and purple so they stand out on the slide. The autopsy showed that
the stent had led to the patient’s fatal blood clot.
Autopsies
should be used to evaluate the effectiveness of other therapies, Virmani said,
from chemotherapy to heart-valve replacements. “The only way to learn is
through autopsies.”
Hospital
autopsies are even rarer when patients older than 60 die in hospitals,
representing a lost opportunity to learn about age-related diseases, Burton
said. More than 684,000 such patients died in hospitals in 2008 — more
than one-quarter of the total deaths in the country — and just 2.3
percent were autopsied, CDC data show.
Without
autopsies to confirm patients’ precise causes of death, public health officials
say, the health-care system overall suffers. Erroneous information sometimes
ends up on death certificates. Broad categories of disease such as cancer are
probably accurate, but specifics such as the type of cancer may not be, said Robert Anderson, chief of the mortality statistics branch of the CDC’s National Center for Health Statistics.
“These data
are used to set public health priorities, to develop public health programs and
allocate resources,” Anderson said. “We do the best that we can given the
information we have, but if you put bad information into the system, you’re
going to get bad information out.”
In 1999, the
Medicare Payment Advisory
Commission, or MedPAC, which advises Congress about Medicare, issued a report
stating that increasing the rate of clinical autopsies could improve health
care and reduce errors.
The report
recommended paying pathologists directly for autopsies and giving hospitals
bonuses or penalties for hitting or missing target autopsy rates. The advisory
group also suggested that Medicare change its hospital regulations to encourage
more autopsies and use them as a standard of performance.
But Medicare has not
acted upon these recommendations. An official from the Centers for Medicare
& Medicaid Services declined ProPublica’s request for an interview, saying
the use of autopsies in hospitals
“is not within
[Medicare’s] bailiwick at all.”
Other
organizations that advocate for better medicine, such as the Institute for Healthcare Improvement,
National Quality Forum and The Joint Commission, have not pushed for higher
levels of autopsies, either, despite the widely held belief that this could produce improved
care.
Raising the rate “is not one of our priorities by any
means,” The Joint Commission’s Schyve
said.
Dr. George
Lundberg, a pathologist and one of the country’s most vocal advocates for
increasing the autopsy rate, shakes his head when discussing the medical
industry’s apathy about low autopsy rates.
Lundberg, the editor of the journal MedPage Today, said The Joint
Commission should re-establish mandatory autopsy rates “like they used to have
back in the good old days of quality when we weren’t running away from trying
to find the truth [about] our sickest patients.”
One way to
shake the complacency, various experts told ProPublica, would be for insurance
companies and the government to pay for autopsies. But an official from
UnitedHealth Group, the largest health-insurance company in the country, said
the autopsy is not reimbursed because it “isn’t a procedure that would prevent
or treat a sickness or injury” in a patient.
Virmani
called this shortsighted. The cost of an autopsy is small relative to the money
spent on drugs, treatment and diagnostic imaging, she said, and the payoff
could save lives and money.
“We are
letting go of something which we could really use tomorrow to improve the
health care of patients,” she said.












