Vascular surgeon Dr. Caitlin Hicks recalls the first time, about a decade ago, that a patient came to her with a lower leg mottled with purple and starting to decay. She searched for a pulse in the damaged limb, but blood had stopped flowing into it.
The patient had previously undergone an invasive vascular procedure, using devices designed to clear out clogged arteries. But when Hicks questioned the patient about the symptoms that had led them to initially seek treatment, they seemed mild or nonexistent.
Then Hicks saw another similar patient, and then another. In some cases, the only solution was amputation.
Over time, she began to worry if the patients landing on her operating table were a harbinger of something more ominous: doctors performing lucrative procedures on patients who might not have needed them.
In clinic offices and outpatient surgical centers, doctors were inserting into leg arteries catheters affixed with lasers or blades to pulverize fatty deposits from vessel walls. The procedures, called atherectomies, carried risks — of infection or the errant nick from a blade — that were perhaps worth the gamble for patients who could lose their legs from poor circulation. But some of the patients Hicks was treating had not initially been that sick.
“A lot of them would tell you, ‘Well, the doctor said I had a blockage in my artery,’” she said, “but if you asked them about symptoms, they didn’t actually have any.”
So Hicks, an associate professor of surgery at Johns Hopkins University School of Medicine, and a team of academic physicians decided to do what regulators and insurers had not. They began years of groundbreaking, peer-reviewed research that revealed that some doctors appeared to be overusing atherectomy procedures, performing them on high numbers of patients who may not have needed them.
They built on studies that showed aggressive, invasive treatments made far less sense for patients with milder symptoms, like leg pain while walking, which is often caused by clogged arteries obstructed with plaque. The majority of these patients are unlikely to develop severe vascular disease, and they can often be treated with less invasive therapies like medication and exercise. While most doctors follow best practices, many have continued to use aggressive interventions, ProPublica found, often warning patients that without them, they could lose their limbs. Instead, research has shown, the procedures may be associated with a higher risk of amputation.
Hicks and her fellow researchers didn’t publicly reveal the outlier doctors, but four years ago, they disclosed their names to the Centers for Medicare and Medicaid Services, encouraging the government insurers to examine their own data and crack down on abuse. They also sent a list to the Society for Vascular Surgery, where senior medical society members and leaders in the field believed the time had come for tighter standards.
And then Hicks and her colleagues waited. Surely their careful, methodical and confidential evidence would prompt change. Instead, what they got was an at-times scalding wave of blowback.
Today, atherectomies remain unchecked, not only because regulators and insurers haven’t done enough to rein them in, ProPublica’s reporting has found, but because doing them remains easy and profitable. Since 2013, the number of atherectomies has doubled and payments to doctors have nearly tripled, totaling about half a billion dollars annually as of 2021, according the most recent year of Medicare data. Physicians can charge Medicare tens of thousands of dollars for multiple procedures conducted in a single office visit.
And the government’s own data shows it continues to pay individual providers millions of dollars a year to perform the procedures, including on patients with only milder symptoms, with little pushback and few rules.
In response to questions, CMS told ProPublica that it examines its billing data for outliers, taking action when it identifies problems by denying claims, suspending payments or referring questionable providers to law enforcement.
But the story of Hicks and her colleagues illustrates the challenges of highlighting potentially dangerous practices and effecting change, especially when physicians’ livelihoods are at stake.
What the researchers hadn’t bargained on was a vocal contingent of doctors willing to fight for their freedom to perform the vascular procedures as they saw fit in their private practices. While not all were outliers, many spent years attacking the overuse studies and the researchers behind them and wielding influence to mute reforms.
Nowhere was this opposition more palpable than this past May, at the annual meeting for the Outpatient Endovascular and Interventional Society, a group of doctors who treat vascular disease outside of hospitals and often in their own private practices. Among glass cases in which atherectomy catheters gleamed like luxury jewelry, hundreds of doctors convened at Walt Disney World’s Coronado Springs resort to learn how to bolster their businesses.
In one presentation, Dr. Sandeep Rao, an interventional radiologist from El Paso, Texas, flicked through a presentation on vascular procedure metrics. “That clinic patient, how well are you in getting to them on the table? And eventually, once you get them on the table, how well you’re converting them into the codes that you can bill for them?” Rao asked the room. “All of a sudden, if that patient doesn’t show up, now again, and that patient just goes, ‘I don’t want any more procedures,’ now that’s maybe something that you may not be able to bill for. So when I have a patient captured and captive on my table, I try to maximize how much I’m able to get.”
(Rao later told ProPublica his comments were focused on patient safety: He wanted to do every procedure necessary at once so that a patient didn’t have to return for a second set of procedures, risking complications.)
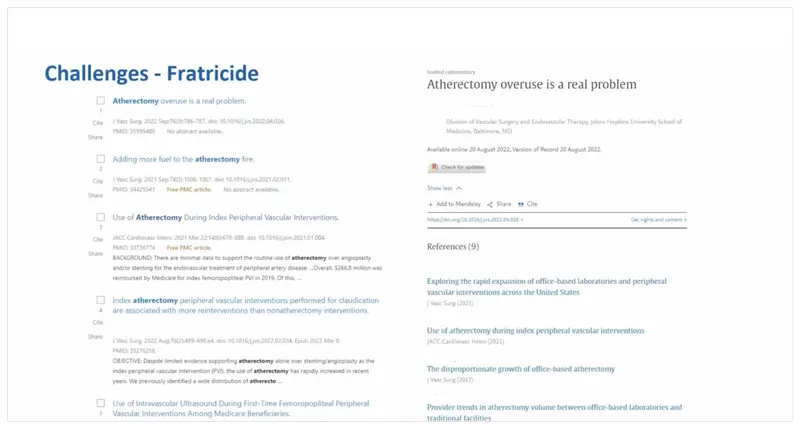
Protecting their practices — both from regulators and critics — was a persistent theme. No physician was perhaps as bold as interventional radiologist Dr. Alex Dabrowiecki of Oregon, who provocatively brandished a slide listing the recent academic articles from Hicks on atherectomy overuse. Stamped at the top in bold letters was the word “Fratricide.”
“There are some academic institutions who find [office-based laboratories] a threat or find big issues with how we are practicing,” he said. (Dabrowiecki later shared with ProPublica that his slide was meant as “tongue-in-cheek.”)
Vascular surgeon Dr. Robert Tahara, who leads the society for outpatient physicians, told ProPublica in an email that his members feel attacked by the research on procedure overuse. “I and many others simply but vociferously take issue with the portrayal that [office-based laboratory] docs are only using atherectomy as a revenue tool,” he said, noting that the Medicare data, used by Hicks and others, has many limitations that “precludes the ability to draw any meaningful conclusions.” Tahara added that terminology used by Rao at the conference was “ill crafted, not well conveyed and does not reflect the OEIS thinking.”
Other private practice doctors have accused Hicks of weaponizing ivory tower research and have vilified her as an “atherectomy nazi.” Some physicians have critiqued the focus on more milder vascular disease, which can have a range of symptoms. Last August, after she published an opinion piece in MedPage Today, which showed that many of her critics are performing atherectomies in the majority of their cases, doctors called on the Society for Vascular Surgery to end her “reign of terror,” threatening a mass exodus if the group did not somehow stop her from continuing her research.
“She will destroy the Society if she is not reined in,” wrote vascular surgeon Dr. Patrick Ryan, founder of the Nashville Vascular and Vein Institute, in a private society discussion board post that was shared with ProPublica, adding that her “abuse of claims data” made private practice doctors a target for regulators. The society later took the post down, citing “personal attacks that were clear violations,” society officials told ProPublica.
“The only result of her work that I have seen is promoting disunion within the [society],” Ryan later told ProPublica in an email, “making me and perhaps others angry that the life and limb-saving work we do every day is being cast as a money grab.”
Ryan, Tahara, Rao and Dabrowiecki did not stand out in a ProPublica analysis of possible atherectomy overuse.
Hicks bristled at the hostility but said her critics misunderstand her motivations.
“I’m just trying to talk about doing the best care possible for patients,” she said. “I’m not trying to suggest that a technology or a practice pattern is evil.”
Outpatient clinics can be an effective place to treat patients and atherectomy procedures are useful in some cases, Hicks said, but she reiterated that some doctors “are doing way too many of these interventions and hastening the worsening of disease in many patients.”


Taking researchers’ mounting concerns of possible patient harm into account, the Society for Vascular Surgery tasked a group in 2018 to develop “appropriate use criteria” to guide doctors on how to treat their patients; these standards are also often used by insurers and regulators to decide which procedures should be covered and which deserve greater scrutiny.
The group determined that patients with milder disease should first be treated with exercise therapy and that invasive procedures should be reserved for those with severe lifestyle-limiting symptoms. In some circumstances, the group concluded, invasive procedures were flat-out “inappropriate.”
But before the standards could be published, the group faced familiar pushback. Some society members attacked the use of the word “inappropriate” to describe some procedures conducted on patients, urging the society to soften the language of the criteria.
“I have no doubt that the publication of this document will result in a huge backlash,” an unnamed society member reportedly said during an internal feedback process. “It will reinforce the perception that the society is trying to rein in the poorly informed, unwashed masses in the community, and protect patients from profit driven surgeons doing unnecessary procedures on their unwitting victims.”
Nearly all 23 authors of the criteria — many of them veteran, highly respected surgeons — wrote to society leadership in February 2022 to defend their process and its terminology, according to an internal letter that was leaked to ProPublica.
“The primary reason to retain the terminology was that the panelists, in fact, felt very strongly that there were certain scenarios that should be deemed as inappropriate,” they wrote. “Simply changing the terms at this point from ‘inappropriate’ to ‘rarely appropriate’ would not only violate the scientific integrity of the project, but [would] also be disrespectful to the extensive work invested by the panelists.”
But two months later, when the society published the criteria, it removed the terms “appropriate” and “inappropriate,” saying that the words have “different and often highly charged social connotations in the 21st century.” They replaced them with the more convoluted jargon “benefit outweighs risk (B>R)” and “risk outweighs benefit (R>B).”
Dr. Joseph Mills, the current president of the Society for Vascular Surgery, insisted that the terminology change didn’t undermine the project’s integrity. “We didn’t change the methodology, we didn’t change the message, we still published it,” he said. Mills, who was one of the authors of the criteria, said he recognizes that overuse is an issue, and that the society would not stop Hicks from doing her research. “We don’t want her to stop doing her work,” he said. “Our true north is always patients first and always try to stick with the science when there is science. I think we’ve been pretty consistent with that.”
But several physicians, including some authors of the criteria, told ProPublica that they felt leadership had caved to the complaints of a vocal minority and made the criteria more vague.
Dr. Rita Redberg, the former chief editor of JAMA Internal Medicine and a cardiologist who has studied vascular disease standards, said such terminology changes can have implications for patient care. “It just leaves a lot more wiggle room and room for interpretation and confusion,” she said. “It’s important to be accurate and scientifically correct. Certainly those kinds of changes for non-evidence based reasons raise a lot of concern.”
Just last month, the European Society for Vascular Surgery published its own practice guidelines, recommending conservative care for most patients with milder symptoms. In contrast to guidance in the United States, it explicitly discouraged routine atherectomy use for patients with milder symptoms, citing the procedure’s “lack of superiority” compared with other treatments, in terms of efficacy and safety.
Some American medical leaders have begun to doubt whether their societies have the capacity to truly address the outliers in their ranks. After former Society for Vascular Surgery president Dr. Kim Hodgson used his platform to call out procedure overuse two years ago, he said in response he was removed from the leadership of a society quality improvement program and projects he had lobbied for to improve care, including an initiative to educate physicians on whether they are outliers, were modified or thwarted.
“I think they have kowtowed to the outliers,” he told ProPublica. “People don’t like to get screamed, hollered and yelled at so they often will appease that group.”
Mills, the current society president, said that Hodgson was not removed from the quality improvement program because of his stance on atherectomies, but because he had retired from practicing surgery and officials wanted a leader who could work more collaboratively with all perspectives. “It wasn’t done to cave in to certain subgroups,” Mills said.
The outlier education initiative that Hodgson lobbied for may still be implemented, said Ken Slaw, the society’s executive director, but so far the society has implemented more voluntary improvement programs. “We could try to make up something like a report card and send it to surgeons and say this is where you lie on the curve of use,” Mills said. “The problem with that is that it makes us a police force.”
Despite the pushback, Hodgson, like Hicks, has not backed down. Standing before dozens of physicians at a conference last month, Hodgson once again appealed to his colleagues that, in the absence of bold society and regulatory action, the onus of protecting patients fell on them all individually.
“We all know who these people are,” he told the doctors. “If you don’t want to be part of the problem, you need to also recognize that part of the problem is the silence.”












