Update, Nov. 21, 2022: On Nov. 18, the Department of Justice and attorneys general for Minnesota and New York filed a notice in U.S. District Court for the District of Columbia stating that they will appeal Judge Carl Nichols’ decision to allow UnitedHealth Group to acquire Change Healthcare. A spokesperson for UnitedHealth said in a statement that the appeal is “entirely without merit” and that the company is “executing on our vision to achieve a simpler, more intelligent and adaptive health system for patients, payers and care providers.”
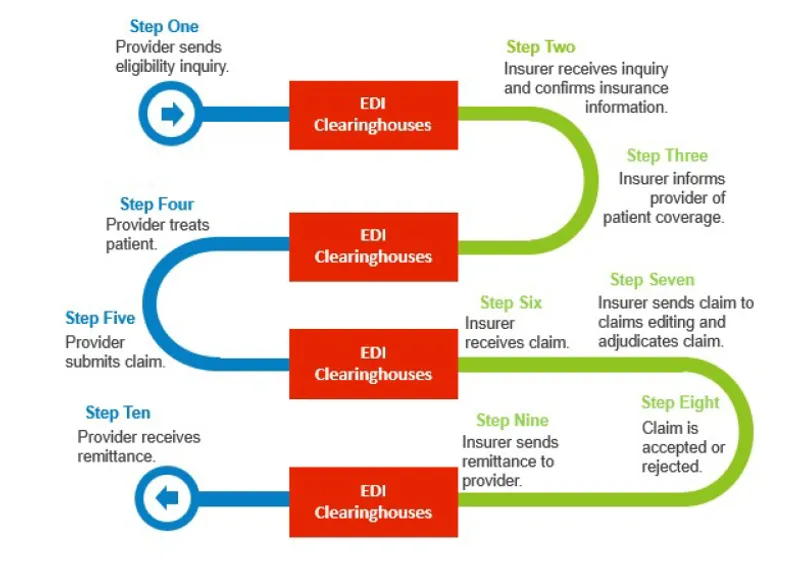
In early 2020, executives at health care behemoth UnitedHealth Group were considering a potential acquisition that could give them the ability to access and analyze a quarter of all medical insurance claims in the U.S. The prospective target, Change Healthcare, was a largely invisible but crucial part of the country’s claims-processing infrastructure — it functions as the pipes that carry insurance claims between health care providers and insurers — and its customers often gave it permission to use their data. What could UnitedHealth Group do with that river of information?
To help answer that question, UnitedHealth turned to McKinsey & Co. The consulting giant concluded that UnitedHealth could “utilize transactions intelligence” from Change’s claims data to “optimize benefit design” for UnitedHealthcare, UnitedHealth’s insurance subsidiary, according to a January 2020 presentation that was cited in a recent lawsuit. That could help UnitedHealthcare, already the biggest health insurer in the country, gain a further edge over its rivals by giving it access to some of the most crucial information in that business: claims data from rival insurers.
UnitedHealth’s deal team cited this type of data use when it presented the potential acquisition to the company’s then-CEO in April 2020. Change’s data could yield “improved medical policy and benefit design” for UnitedHealthcare, the deal team wrote in a subsequent memo. The data could also help UnitedHealthcare track the pricing of medical procedures and expand insurance underwriting. There was just one problem: Using Change’s data in some of these ways could raise “antitrust concerns,” according to an internal UnitedHealth document.
That observation was prophetic, and it would become public through an antitrust suit. UnitedHealth announced plans in January 2021 to buy Change for $13 billion. The press release announcing the deal predicted the merger would “enhance” the services offered by both companies “with insights drawn from billions of claims transactions.” The Department of Justice, along with attorneys general for Minnesota and New York, sued to block the transaction. The case went to trial this summer, and on Sept. 19, Judge Carl Nichols of the U.S. District Court for the District of Columbia decided the suit in UnitedHealth’s favor.
Unless the Justice Department decides to appeal — it faces a deadline of Friday — the judgment will shape the competitive landscape of the U.S. insurance industry and, according to the government, could raise costs for other health insurers in the future. Those price increases, presumably, would get passed on to consumers. But the trial itself turned on the very question examined by McKinsey (which didn’t respond to a request for comment): What might UnitedHealth do with Change’s data in the future?
Even after being presented with evidence that UnitedHealth had discussed using Change’s data to gain a competitive advantage, the judge accepted UnitedHealth’s claims that the company would never do such a thing. His 58-page opinion dismissed the McKinsey documents as “mere references to data and data rights” and concluded that UnitedHealth’s history of compliance with its own rules on maintaining data firewalls, along with the “convincing testimony from senior executives,” were persuasive. The evidence “does not reflect a single instance in which these firewalls have been breached,” the judge wrote after a two-week bench trial. Nichols found that, for the government’s claims to be true, UnitedHealth “would have to uproot its entire business strategy and corporate culture; intentionally violate or repeal long-standing firewall policies; flout existing contractual commitments; and sacrifice significant financial and reputational interests.” He concluded that the Justice Department had failed to show that UnitedHealth would “take such extreme actions.”
The judge’s opinion largely echoed the company’s positions. At trial, for example, UnitedHealth’s lead attorney criticized the Justice Department for failing to “identify a single instance” in which the company used competitors’ data to give its insurance subsidiary an edge. UnitedHealth asserted that it has a long history of abiding by strict firewalls that prevent unauthorized use of data, and CEO Andrew Witty testified that asking UnitedHealth’s data analytics unit, OptumInsight, to share information about insurance competitors with UnitedHealth’s insurance arm “would be against the tone, the culture, the rules, everything we stand for in the organization.”
For its part, the Justice Department pointed to internal company records like the McKinsey presentation and subsequent executive emails to cast doubt on such assertions. Another internal document appeared to downplay the significance of the firewalls between Optum and UnitedHealthcare. “We need to stop thinking that just because we need to have financial and data firewalls between Optum and UHC means we can’t show up together and harness the capabilities of both organizations together,” an unnamed senior executive wrote in a February 2021 memo. “We need to take a deep look at how success is defined for each operating unit.”
At trial, UnitedHealth denied that these documents revealed the company’s intentions and derided the Justice Department’s arguments as a “daisy chain of speculation.” The company, which declined to answer most of ProPublica’s questions on the record, has previously said that the merger will be “good for all participants in the health system, especially consumers” because it will help UnitedHealth “reduce the high costs and inefficiencies that plague the health system.”
Beyond the evidence considered at trial, it’s clear that data analytics are central to a sweeping vision laid out by Witty to place UnitedHealth at the center of almost any health care transaction in the U.S. Witty said at UnitedHealth’s annual investor conference last year that the company needs to “continue to appropriately understand the data we’re privileged to hold and make sure that we can connect people more effectively” to UnitedHealth’s products and services. That will depend on “fantastic internal collaboration” between its data analytics arm, Optum — the unit acquiring Change — and UnitedHealth’s insurance arm, UnitedHealthcare. The goal, Witty said, is to expand UnitedHealth’s customer base from 45 million to 330 million Americans. That’s basically everyone in the U.S.
Witty used the hypothetical example of an uninsured 28-year-old who goes online to buy Advil from UnitedHealth’s internet pharmacy and then ends up consulting a UnitedHealth doctor for knee pain, getting a UnitedHealth loan to get a knee replacement at a UnitedHealth surgery clinic and eventually buys health insurance from UnitedHealthcare. “And that’s really the future of the company,” Witty said.
There was another issue, unexplored at the trial, that seems relevant to Witty’s testimony about “the tone, the culture, the rules, everything we stand for in the organization”: His company’s lengthy history of questionable practices.
In recent years, for example, UnitedHealthcare has been accused of sweeping billing irregularities in Medicare Advantage plans. Last year, it was accused of extracting $3.7 billion from Medicare by manipulating beneficiaries’ health risk assessments, according to a September 2021 report published by the Department of Health and Human Services’ inspector general. (The report cited similar behavior among other insurers, but it found that one company “stood out from its peers”; the agency later identified UnitedHealthcare as that company. UnitedHealth asserted at the time that the report was “based on old data” and called it “inaccurate and misleading.”)
And in 2017, the Justice Department joined two whistleblower suits alleging that UnitedHealthcare knowingly ignored information about beneficiaries’ medical conditions to inflate payments it obtained from Medicare. The government alleged that UnitedHealthcare received at least $1 billion more than it should’ve received. One of the two cases is still in litigation; the other was dismissed in part because the alleged wrongdoing occurred too long ago. UnitedHealthcare denied wrongdoing in both cases.
UnitedHealth’s pharmacy services arm has faced similar complaints. In late October, OptumRx reached a $15 million settlement with Ohio’s attorney general for allegedly overcharging the state to provide prescription drugs to Ohio’s Bureau of Workers’ Compensation. (OptumRx admitted no wrongdoing in its settlement with Ohio, which is seeking similar recoveries from other companies.)
And more than a decade ago, UnitedHealth’s data practices ran afoul of authorities, who concluded the abuse led to higher prices for consumers. A 2008 investigation by New York’s attorney general found that UnitedHealth’s Optum data analytics arm, then known as Ingenix, let health insurance companies manipulate a database used to establish reimbursement rates for their members’ out-of-network medical expenses and that “UnitedHealth Group itself participated directly in the manipulation of the data.” A Senate investigative panel concluded in 2009 that Ingenix allowed insurers to scrub their data submissions to eliminate high charges, thus allowing them to reduce their payouts and shift the burden to customers. “The result of this practice is that American consumers have paid billions of dollars for health care services that their insurance companies should have paid,” according to a 2009 Senate staff report. UnitedHealth executives admitted in Senate testimony that the company’s ownership of Ingenix’s benchmarking database created a conflict of interest. They agreed to offload the data to an independent nonprofit as part of a settlement with New York.
Antitrust challenges tend to focus on narrow theories of potential competitive harm caused by a merger — like the assertion that UnitedHealth could use its new claims data to feed competitive intelligence to its insurance business. So prior history that doesn’t exactly match those theories tends to get left out of the litigation, according to Erin Fuse Brown, a professor of law at Georgia State University who specializes in health care law. Still, UnitedHealth’s history suggests “it’s clear that they are finding ways to use data to make money,” Fuse Brown said. That applies to the Change Healthcare deal, she said: “You have to wonder: What is the value proposition? Why is United spending so much money to buy this company?”
Wall Street seems to have viewed UnitedHealth’s recent ambitions through that prism. Since the merger was first announced on Jan. 6, 2021, UnitedHealth’s stock has far outpaced the broader stock market, rising 46% vs. 17% for the health care sector and 7% for the S&P 500. JPMorgan Chase analysts predicted in a research note that insights from Change’s data will benefit UnitedHealth’s insurance arm as well as Optum’s other customers. Analysts at Deutsche Bank were more sweeping. They called UnitedHealth’s courtroom victory a “positive leading indicator” for more consolidation in the health care sector, according to a September research note.
The Justice Department has no easy options after its courtroom defeat. Appealing the decision risks underscoring the extent of its defeat if the agency loses, though it would emphasize the Justice Department’s willingness to fight. Otherwise, the department may choose to save its powder for another battle. UnitedHealth finalized the acquisition of Change two weeks after the judge ruled in its favor, making the acquisition an accomplished fact and thus difficult to disassemble.
Mergers like UnitedHealth’s acquisition of Change are the toughest to tackle, even for a Justice Department that has become more willing to challenge mergers under its current antitrust chief, Jonathan Kanter. So-called vertical mergers — those involving companies with different roles in a production process — have long been the hardest to block. “There was a lack of case law and whatever case law existed wasn’t favorable,” said Thomas Greaney, visiting law professor at the University of California Hastings College of the Law. As a result, vertical merger challenges “became very difficult cases to win and hence the enforcers didn’t bring many of those cases,” said Greaney, who studies antitrust enforcement in the health care sector.
Antitrust enforcers at the Justice Department and the Federal Trade Commission have instead largely focused on so-called horizontal mergers, which involve direct competitors merging within the same industry. Such mergers have long been presumed to be anticompetitive when they involve two big competitors whose combined market share would be dominant. For that reason, antitrust officials have had success in challenging mergers of hospitals serving the same region. The Justice Department enjoyed a recent high-profile courtroom victory in blocking a proposed horizontal merger in the publishing sector between Penguin Random House and Simon & Schuster, and four other horizontal deals have been abandoned when the agency filed a complaint or on the eve of it filing an antitrust complaint.
Vertical mergers, which are becoming more common in the health care industry, are not treated by courts as presumptively anticompetitive. Courts are more skeptical of claims of competitive harm that might result from a hospital operator buying, say, a chain of physician practices. But evidence emerging from academic studies shows that vertical integration in health care can drive up prices for consumers as well.
Greaney said it will take time for courts to rethink their approach to vertical tie-ups like UnitedHealth and Change. How long? “It’s turning around the oil tanker in the ocean,” he said. “You give the command, but it takes quite a while to move the law.”
Disclosure: McKinsey is a sponsor of ProPublica events.
Mariam Elba contributed research.