Marty and Candy Larsen were in their pajamas, getting ready to watch a movie in the living room, when they heard their 27-year-old daughter scream.
“I need help!” Julia cried.
They could see her standing just a few feet away, her long blond hair unkempt, her blue-gray eyes at once alert and vacant. She’d looked like this in other moments when fear overtook her and reality slipped away. But a new sight jolted them upright: their daughter’s fingers, wrapped around a pink handgun.
Julia pounded the weapon against a wall, then squeezed its trigger, sending a bullet down an empty hallway. “Help me!” she shrieked.
The parents scrambled in different directions. Candy was on with 911 while Marty reached toward his daughter. “Julia, stand down,” he said. “How can we help you if you don’t stand down?”
But Julia fired again, repeating her plea like a mantra.
“Help me!” she cried. “Help me!”
The need had been building for almost six years, since she returned home from a stint as a Navy firefighter aboard a warship in the Persian Gulf. She was tormented by the rippling trauma of an on-duty sexual assault and grappling with symptoms that led her to be diagnosed with a psychotic disorder.
She was dependent on the Department of Veterans Affairs for care. Just that morning, when her latest crisis began, a nurse at the local VA clinic in Chico, California, had told her mother to bring her in. When they arrived, a telehealth provider was too busy to see Julia. A social worker asked questions to gauge her risk of suicide or violence; even though Julia refused to answer, she was sent out into the world and told to return for the next available appointment, in 11 days.
Such dysfunction had become the norm at the Chico clinic, one of several hundred such community facilities designed to serve veterans who live far from the nation’s big cities. From the outside, it looked like a haven for heroes: a state-of-the-art building with a gleaming atrium, a large American flag flying out front. But the clinic hadn’t had a full-time, on-site psychiatrist in five years. A single nurse was responsible for connecting hundreds of veterans, some with serious mental illness or active suicidal thoughts, with an ever-changing lineup of telehealth providers in different time zones.
The military has long drawn recruits from remote towns across America, promising them a lifetime of health care in return for their service. But the VA has seldom staffed those same communities with the mental health professionals needed to help them once they return home. Two decades of war in Iraq and Afghanistan have turned this chronic shortcoming into an emergency. The demand for mental health care has grown at a rate that’s triple the rate of growth for all VA medical services. Anguished employees, doing what they can with threadbare staffing and glitchy technology, are burning themselves out trying to avert disasters that feel inevitable. In Chico, nurses and social workers cried after their shifts, and the new site manager, a veteran and longtime health care administrator, had made a grim prediction: “We are going to kill someone,” she told colleagues.
If hindsight is 20/20, agency officials should have exquisite vision by now. Their files are littered with cautionary tales of missed screenings and insufficient follow-up; in at least 16 instances since 2019, veterans who received inadequate care wound up killing themselves or other people; an additional five died for reasons related to the poor quality of care. Each time, investigators with the VA’s Office of Inspector General swooped in to determine whether the system failed; each time, they concluded it had.
To plug the holes, the VA grew its nationwide mental health workforce by more than 4,000 last year and plans to hire an additional 5,000 professionals over the next five years. But the sense of dread lingers. It’s a “perfect storm of real potential for gaps in care,” said Alyssa Hundrup, a director on the Government Accountability Office’s health care team.
Just as violence was erupting in Julia’s home on Jan. 3, 2022, another veteran sat alone in his dark bedroom, not far away, ruminating. Deep circles hung below his eyes. An unruly beard covered his chin.
Andrew Iles, 33, had come to believe the government was monitoring him and that his mother was in on the conspiracy. He, too, had tried to get help at the Chico clinic but for years was passed from provider to provider. Recently, all he could get was a psychiatric pharmacist who prescribed him pills. He felt abandoned, concluded the VA had never wanted to help him and slipped into a state of paranoia so intense that he threw away his belongings and holed himself up inside his mother’s house.
His sister, once his protector and closest ally, had stopped bringing her family to see him. His mother had tried to remove all of the firearms from the house but missed a few. Andrew had stowed them away.

Chico, California, sits in the northern Sacramento Valley, in the shadow of the Sierra Nevada mountain range. It’s a college town home to museums and breweries, funky cottages and trendy restaurants. Climb into the foothill elevation, though, and you enter another world. Aside from some big-box stores and picturesque downtowns, it’s mostly wilderness dotted with private homes. Cellphone service is spotty. Roads snake through dense forests.
Andrew Iles grew up in a particularly isolated community called Concow. When he was a kid, only a few hundred people lived there. They drove the same mountain roads, shopped at the same convenience store. There were enough children for a small school, but each grade level had just a handful of students. Most were eligible for free lunch.
Andrew’s family lived a mile off the main road in a one-room, A-frame home that sometimes had no electricity or running water. His parents, Glen Iles and Sue Hill, used methamphetamines. They disappeared, often for days at a time, and let other drug users hang around the house. Some of them forced Andrew and his big sister, Ashley Hill, to engage in horrific sex acts. The kids stayed quiet about the abuse. “We were so afraid to say anything,” Ashley recalled.
The siblings sought refuge on the mountainside. It was their own wild playground, full of creeks to splash in and salamanders to chase. But violence was never far. Once, when Andrew and Ashley were in grade school, they found their mother handcuffed to a refrigerator, bleeding from three gunshot wounds. A few years later, they watched Glen hold Sue at gunpoint and threaten to shoot her. Ashley called 911. Glen fled into the forest on his ATV but was caught and sent to prison. The ordeal made the local newspaper.
The arrest was a turning point. Sue stopped using drugs. She found a new partner and moved the family a few times, ultimately settling in a small city in the foothills called Oroville. After finding steady work at a rent-to-own furniture store and a new place to live, she started rebuilding her family.
Andrew grew into a gangly teenager with a sly sense of humor who wore braces, dyed his hair bright colors and swept his long bangs across his face. He and his friends were emo kids; they listened to Fall Out Boy and spoke out against the war in Iraq. Andrew dated the same girl for years. He showered her with attention and wrote her silly notes. He put considerably less effort into his schoolwork. As graduation neared, he started to believe he needed structure and discipline, and he thought the Air Force might provide it. Plus, he had a mind for math and technology, and the idea of working on multimillion-dollar airplanes appealed to him. “If I don’t do something like this,” he told his mother, “I’ll be in Oroville for the rest of my life.”
As a new airman, Andrew was stationed in Arizona as an aircraft electrical and environmental systems apprentice. His supervisors rated his performance as “truly among the best.” His first evaluations touted his “unrivaled initiative” and described him as a “superior performer” and “stellar airman.” One evaluation ended with a simple declaration: “Promote now!”
Andrew raised his hand for an assignment on Kunsan Air Base in the Republic of Korea where he could work on F-16 fighter jets. He traveled the country by train, visiting university cities so he could meet people his age. He found it thrilling to be somewhere so different from Concow with such freedom to explore.
His next tour took him to Ramstein Air Base outside Frankfurt, Germany, to work on hulking C-130s. He was 22 then, excited to visit Berlin, Amsterdam and Paris. But he was increasingly looking over his shoulder, wondering what his peers were saying about him.
Around that time, Andrew sent emails to his mother and sister that described neighbors spying on him. Sue and Ashley found the letters troubling. In some ways, Andrew sounded like his father, who had never been diagnosed with mental illness but was prone to paranoia and conspiracy theories.
Andrew had reached the age when, experts say, a typical life can start to veer off course. It is generally believed that some people have a greater biological risk of developing psychotic disorders than others. Genetics can play a role. Environmental factors like stress can trigger the onset of illness or make it worse than it would have been. Symptoms tend to begin when people are in their late teens or early 20s, as their brains mature.
Andrew sought out behavioral health services on the base, he said. But he was certain his bosses saw him differently after that. He felt some treated him like he was less capable, while others seemed to think he was faking. He considered ending his life.
In late 2010, long before Andrew was supposed to leave Germany, he wrote his commanding officer saying he no longer believed he could do his job and asking to leave the military, he recalled. The Air Force approved his request for separation, giving him an honorable discharge, records show, but required him to transfer his remaining active duty service to the reserves, he said.
When asked about the circumstances of Andrew’s separation, an Air Force spokesperson, Michael T. Dickerson, said he could not comment on anything related to an individual’s physical or mental health or the nature of his or her discharge.
Andrew flew back to the United States. He was active in reserves in northern California for a period. But his growing fears about government surveillance kept his mind in constant motion. At night, he thought he could hear strangers talking about him through doors and windows. By 24, he’d moved back in with his mom and stepdad in Oroville, the one place he’d dreaded ending up.



Julia Larsen grew up a 40-minute drive from Andrew in a quaint foothills town called Paradise. Her father worked for the post office. Her mother ran a home day care. The youngest of three daughters, Julia was bound by few rules. She spent most of her time outdoors, searching for animals or digging in the red earth. A treasured family photo shows her holding a catfish she reeled in herself.
People who knew Julia as a teenager describe her as bubbly and a free spirit. Her senior superlative in high school was “biggest daredevil.” Her family was always camping or hiking together. On weekends, when her friends came over for backyard sleepovers, her mother often joined them around the campfire. In Julia’s mind, Paradise lived up to its name. But like many young people, Julia was eager to escape the place she was from. So one day, she and some girlfriends struck up a conversation with the local Navy recruiter.
Julia told her parents while the family ate dinner together at the kitchen table. Marty, a Navy veteran with an anchor tattooed to his forearm, was elated. “I couldn’t stop bragging about her,” he would later recall. Candy worried about Julia’s safety overseas but trusted her to make the right decision. The two were more like sisters sometimes than mother and daughter.
Julia arrived at boot camp outside Chicago in June 2012. She was 18. She traded a colorful sweater and jeans for a Navy-issued T-shirt and shorts and lined up to have her hair cut. The recruits marched and swam and studied and shot. It was easier than she expected. Her parents and middle sister came to watch her graduate. They cheered from the bleachers and then celebrated over deep-dish pizza and White Castle hamburgers.
When it came time to specialize, Julia became a flight deck firefighter. She went for additional training in the Florida Panhandle, where she learned to work a high-pressure hose and handle rescue equipment. That fall, she was assigned to the USS Theodore Roosevelt, an aircraft carrier undergoing major upgrades near the Naval base in Norfolk, Virginia. Her home was a cramped bunk with a flimsy mattress deep in the ship’s belly. She placed the few personal possessions she had in a tiny locker and reported for duty.
She doesn’t remember much about the first day or even the first week. But she remembers the comments a supervisor started making about her body, and the way he pressed himself against her when she was chopping lettuce for the salad bar. Later, while she was on dishwashing duty in the ship’s scullery, he approached again, she said. He grabbed her arms and folded them across her chest. Unbuttoned her top. Turned her around. He was bulky, much taller than her 5-foot-7-inch frame, and had a thick, dark mustache. Julia had never felt so helpless. She fought to free herself from his grasp, burning her right wrist on a hot dishwasher in the struggle, but was completely overpowered. Before he could get much further, another young sailor walked in. The supervisor got spooked and scurried out.
Julia told a friend. Then she told the team that handled sexual assault allegations, she said. She wasn’t afraid of repercussions. She had been so excited to enlist. Was this what the rest of her military experience would be like? The Navy gave her the option to transfer to a different ship. For Julia, it was an easy call. She no longer wanted to be on the Roosevelt.
But while the Navy offered Julia a fresh start, it didn’t offer her mental health services, she said, as Department of Defense policies demanded. “I would have taken them up on it,” she told ProPublica. Asked to respond, a U.S. Navy spokesperson said, “While we cannot comment on the care Ms. Larsen may or may not have received, the Navy takes mental health for our Sailors seriously.”
It was, experts said, a crucial missed step. Research shows a clear association between military sexual trauma and mental health conditions including post-traumatic stress disorder, depression and suicidal ideation. Studies have shown treatment can help reduce PTSD and depression symptoms, which sometimes emerge years after the traumatic event.
Julia was assigned to the USS Kearsarge, a massive assault ship that was already in the Middle East to support troops in the global war on terrorism. During her second deployment to the region, in the spring of 2016, a Harrier jet burst into flames departing from the Kearsarge’s flight deck. Julia was startled by the deafening pop. She sprinted toward the burning aircraft with the other firefighters to battle the blaze. “Her initial response, quick action and knowledge during an AV-8B Harrier fire on the flight deck was pivotal in the prevention of a major catastrophe and loss of lives,” her supervisors wrote in her performance evaluation.
Almost four years to the day after she began boot camp, Julia returned to California. She moved into a house in the southern Central Valley with her boyfriend from the Navy and enrolled at the local college. She set a goal of earning a degree in social work and becoming someone who could help veterans. But Julia couldn’t shake the feeling that something was wrong. She had trouble concentrating on schoolwork. Some nights, she couldn’t sleep. She sought out counseling through the VA.
By June 2017, Julia had started feeling scared of the world around her. One night, she was certain she could hear people walking on her roof and called the police. The officers who showed up made her feel even more anxious. She worried they would take advantage of her. She pushed one and wound up at the police station. She was later taken to a psychiatric unit.
As soon as Marty heard what happened, he drove six hours to pick up his daughter. He packed her belongings into suitcases and hitched her car to the back of his truck. On the ride back, Julia was convinced they were being followed. She begged her father not to draw attention by driving too fast or changing lanes. Marty was stunned to see his easygoing daughter acting so out of character. “It was like a switch had flipped,” he recalled.




For veterans in the foothills like Andrew and Julia, the Chico clinic was all they had.
Its mental health team had been trying for years to convince regional leaders to add more positions. Even when the staff included two psychiatrists and a psychologist, plus a nurse, counselor, social workers and designated mental health administrators, the team struggled to keep up with growing demand, former employees told ProPublica. The clinic had more than 500 mental health patients, many of whom had complex illnesses.
The department’s longtime manager, a psychiatrist named Russell Cottrell, recalled once noticing that other rural mental health departments in the region had more personnel per patient than Chico did, he said. When he asked about the discrepancy, his bosses stopped sharing the data. He fumed, he said.
“I don’t think they paid attention to the growth we had,” Cottrell told ProPublica. “I would point it out and I’d get in trouble.”
By the summer of 2016, the staff had gotten smaller, and Cottrell was the only psychiatrist in the building. Cottrell was no stranger to hard work; an Army veteran, he had devoted his career to treating the most challenging mental health cases. But he was tired of begging for personnel and running out of energy. That fall, he made plans to retire.
The lead mental health nurse, Michelle Angela, sent an email to a regional mental health leader in the wake of Cottrell’s retirement announcement. “We would like to invite you to come visit us at Chico Behavioral/Mental Health for an update on what the plan will be,” she wrote. “In addition to our concerns as staff members, our local veterans have been asking if there will be [a medical doctor] on site for their mental health needs.”
No such doctor was hired. Instead, the clinic filled the gap with a combination of visiting doctors and doctors in other locations who connected with patients through computer screens.
In many ways, the Chico clinic was on the forefront of telepsychiatry, then an emerging way to deliver treatment that had the potential to broaden access to veterans in remote locations. But some mental health professionals had reservations. While virtual sessions might work for some patients, they worried others needed the trust and connection that could only be established in person.
For Andrew, who started coming in for treatment after his father died in 2013, the changes were disorienting. Andrew had been seeing Cottrell and starting to untangle his thoughts. When Cottrell retired in February 2017, Andrew was assigned to a temporary doctor, then a specialized pharmacist who wrote prescriptions, he said. Andrew resented the arrangement. “I wanted to talk to someone routinely,” he said, “not just get a load of meds.”
Julia first arrived at the clinic on June 23, 2017. She wouldn’t maintain eye contact with anyone; while in the waiting room, she rearranged the chairs. That day, clinic staff offered her little in the way of answers. “She was informed that Chico VA Behavioral Health is an outpatient clinic and we do not have a psychiatrist on site,” a social worker wrote in her medical records.
The following month, Julia started coming into the clinic for telehealth appointments with an off-site provider. Her records show she was diagnosed with PTSD from combat and military sexual trauma and bipolar disorder, the latter of which she disputes.
For a while, the patchwork system in the clinic’s mental health department seemed to be working, current and former employees told ProPublica. But cracks started to show. In 2018, the psychologist left. And the clinic sometimes found itself without a telehealth provider available to refill medications or see patients in crisis, emails obtained by ProPublica show.
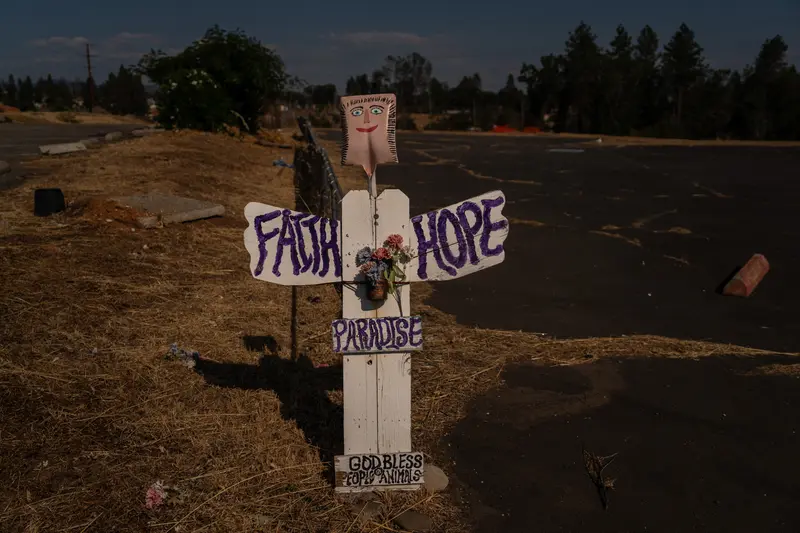
That November, a wildfire started burning up in the foothills. It was called the Camp Fire because it originated off Camp Creek Road. The blaze grew into a raging inferno that affected virtually everyone in the region. More than 10,000 homes were destroyed, including the one belonging to Marty and Candy Larsen where Julia grew up. At least 85 people died.
The day after the fire, when the air was still heavy with smoke and ash, Cottrell showed up at the clinic to help. He knew the fire would increase the demand for mental health services, he said. Seven months later, he came back on a part-time basis to help out until the clinic could hire a new full-time psychiatrist on site.
Months passed without a hire. Meanwhile, the Chico clinic moved into a gleaming new facility just a few miles away. The VA’s website trumpeted its status as a green building with energy-reducing and cost-saving features. But none of that improved the mental health department, former employees said. In fact, the new building eliminated a designated waiting area for veterans in crisis as well as private offices for mental health practitioners, meaning patients were seen in bare-bones exam rooms that evoked a school nurse’s office.
Amid the turmoil, Andrew struggled. When he noticed Cottrell back in the clinic, he wondered if Cottrell hadn’t really retired but had discarded him as a patient. Experts who were not involved in Andrew’s care told ProPublica that the constant provider changes would likely have reinforced Andrew’s paranoia and made him feel less connected to his care. One said the churn would have felt like a parent continually rejecting their child.
Julia’s life had become a rollercoaster. Some days, she felt great. She enrolled at Chico State and floated around its red-brick campus. “She could be very lucid and be her old self,” Marty recalled. “We kept thinking, she’s over it.” But stressors would trigger her. She would flash back to her darkest moments, start feeling paranoid. It wasn’t unusual for her to go days without sleeping.
She wanted counseling, she told ProPublica. But at the clinic, there was never enough time to get into it all. The focus seemed to be more on medication than talk therapy, she said. “They wanted to help me and [then] shoo me along,” she said.

The strain on the clinic would only get worse.
The same month that COVID-19 swept across the country, the mental health team learned its designated administrative assistant would be shared by several departments. That made managing appointments even more difficult. Not long after that, one of the two telepsychiatrists started seeing fewer Chico patients.
Cottrell had had enough, he said. He decided he would retire for good at the end of the year. “I saw it as a lost cause,” he told ProPublica.
That summer, a psychiatrist on the East Coast was hired to do virtual visits on a part-time basis. But increasingly, technical problems were disrupting appointments.
In emails to regional mental health leaders, Chico’s front-line workers insisted that hiring an on-site psychiatrist should be the priority and noted the VA’s own guidelines, which said veterans who were suicidal, violent or in need of immediate medical attention should not be referred for telehealth services. “We currently have numerous serious suicidal ideation patients,” a nurse named Diana McMaster wrote. “With losing Dr. Cottrell, do we not need a psychiatrist in the building? A lot of times it is left up to Michelle and me to manage what happens with these patients on our side of the video. … That puts us in a precarious position.”
Dr. David Gellerman, the chief medical director for mental health services in the VA’s Northern California region, replied, writing, “No, we are not placing anyone in a precarious position. We can’t hire someone who does not exist… if we get a good psychiatrist or [psychiatric nurse practitioner] candidate who can be on location, we can try, but so far we have not had any acceptances.”
Gellerman pointed out that precautions were being relaxed in the pandemic. “Care by telehealth is better than no care at all,” he added.
Reached by email by ProPublica, Gellerman did not comment on the correspondence. He referred a reporter to the VA’s public affairs office that covers the broader region of Northern and Central California, Nevada, Hawaii and the Philippines, which did not respond. A national spokesperson said agency guidance does not establish absolute conditions under which virtual care should not be given.
By then, Andrew had been diagnosed with schizoaffective disorder, a mental illness marked by a combination of schizophrenia and mood disorder symptoms. People with the disorder can experience psychotic symptoms, losing their connection to reality.
Andrew hadn’t been employed since returning to Oroville. He had come to believe people were trying to kill him, even his family. He spent most of his time alone in his bedroom. He slept upright in his computer chair and ate only food that came in a can so nobody could poison him.
Sue quit her job to care for her son. She made sure he had canned food to eat and drove him back and forth from his VA appointments. In conversations with her sister, Sue worried Andrew’s doctors were always changing and he wasn’t getting the help he needed. Ashley felt helpless watching her little brother slip away. He was withdrawn and angry, a far cry from the outgoing kid she remembered. She thought back on how she had tried to protect him when they were children. “It felt like I’d failed,” she said.
The pandemic had rekindled Julia’s paranoia, too, so much so that she began to believe strangers wanted her dead. That May, her oldest sister, Jordan Pepper, a clinical mental health counselor in Ohio, traveled to Chico and helped her to seek in-patient treatment at the VA hospital near Sacramento, California. Doctors there diagnosed her with general psychotic disorder.
Records show Julia went to the Chico clinic in the weeks and months that followed. Candy and Marty took turns accompanying her. Candy made it a point to get to know the people who cared for her daughter, in some cases getting their personal cellphone numbers. She tried to stay optimistic.
In the fall of 2021, the telepsychiatrist who had been seeing Julia stopped seeing Chico patients. That November, Julia had a virtual appointment with a psychiatric nurse practitioner she had never seen before who prescribed a drug called atomoxetine to help her concentrate, her medical records show. But two days later, Julia called back and asked for something that would work faster. The nurse practitioner prescribed an antidepressant called bupropion and instructed Julia to take the two medications together, her records show.
More than a year later, in its report on Julia’s case, the VA’s inspector general would note that the combined use of atomoxetine and bupropion can trigger psychotic or manic symptoms. The nurse practitioner told investigators that despite what his notes said, he had not intended for Julia to take both. It isn’t clear which, if any, Julia took. She doesn’t remember.
Around that time, Julia began taking note of unusual things she believed were happening to her: strangers following her at the dog park, electronic files going missing. She installed a camera in her car and started carrying a pink handgun she bought after separating from the Navy.
The Chico clinic’s mental health department, meanwhile, fell further into disarray, current and former employees told ProPublica. Several other telehealth providers left, including the Connecticut-based telepsychiatrist who was seeing Andrew. Those who stayed buckled under the weight. “We were abandoned,” said Belva Fay, a senior social worker who was also the clinic’s acting manager for eight months. “We were trying to run a clinic with nobody to prescribe medications, nobody to see emergency cases, nobody to talk to these clients who are angry. …
“We kept saying, there is going to be a problem,” Fay said. “This is going to blow up.”
By the time Michelle Gradnigo started as the clinic’s site manager in October 2021, disaster felt all but certain. Gradnigo, a retired lieutenant colonel in the Army and longtime military health care administrator, was so troubled by the lack of on-site mental health care providers that she asked if the clinic’s primary-care physicians could handle some of the load, she said. The answer was no, she recalled.
“I reached out to anyone at the time who would listen and said we are going to kill someone,” she told ProPublica.

VA officials told ProPublica the Chico clinic was trying to recruit mental health professionals by offering special salary rate increases, education debt reduction and relocation incentives.
Northern California VA leaders were also trying to grow the virtual mental health program. A proposal obtained by ProPublica through a Freedom of Information Act request shows that mental health vacancies were dogging clinics across the region and that “painstaking and time-consuming recruitment efforts” were bearing little fruit. The only positions drawing quality applicants, according to the presentation, were virtual.

When the sun rose over the Sierra Nevada mountains on the third morning of 2022, Julia’s eyes were already open.
She had been awake for days, a fact she blamed on what felt like a constant barrage of electric shocks. She had tried to stop them by covering her walls in aluminum foil, but it wasn’t helping. She wanted pills to calm her down. At 8 a.m., she left a message at the clinic that she was “in crisis and very anxious,” government records show. An hour later, she started texting her mother, who called the clinic in tears. The mental health nurse was home that day with COVID, so a nurse from another department took the call.
The nurse sent an instant message to Julia’s nurse practitioner, who was seeing patients from another location, asking if Julia should come into the Chico clinic or go to the VA hospital in Sacramento. The nurse practitioner wanted Julia to go to Sacramento, government records show. But the nurse misunderstood and told Julia’s mother to bring her to Chico.
Marty and Candy brought Julia to the clinic around 2:30 p.m. Her body was tense, her eyes red and heavy with tears. But the nurse practitioner never evaluated her. He had nine appointments that day and no time to see Julia, a violation of VA policy requiring same-day availability for patients in crisis.
A triage social worker tried to ask Julia questions to help determine her risk of suicide or violence, but Julia wouldn’t engage, records show. Instead, she quibbled with her diagnoses and voiced frustration over the recent change in her mental health provider. The social worker should have posed the questions to Julia’s mom, who was inside the clinic while Julia’s dad waited in his truck. Instead, she marked Julia’s disposition as “routine” and concluded she wasn’t a threat to herself or others. There is no indication the social worker asked about Julia’s access to guns or other lethal means.
Later, in an interview with the inspector general’s office, the social worker said she was unfamiliar with the protocols. She ultimately gave Julia the nurse practitioner’s next available appointment, in 11 days.
Julia stormed out of the clinic, furious that she had not been given the medication she wanted, her father recalled. Candy was frustrated; she wanted clear direction on how to help. Exhausted, they all headed back to Candy and Marty’s home, a cozy ranch on a remote hillside outside of Red Bluff, California.

Back at home, Candy offered Julia some soup and a sandwich and tried to help her calm down. Julia was still agitated, but around 10 p.m., she took a sleeping pill and retired to her parents’ bedroom. When it was quiet, Candy and Marty got ready to watch a movie in the living room, hoping it might help them relax.
Just before 11 that night, a call came into 911 dispatch.
The recording captured Julia as she pleaded for help, then fired one gunshot, then another. The line stayed open for an hour, chronicling all that unfolded.
After the second bullet fired into nowhere, Candy was determined to lower the temperature. “We are trying to help,” she assured her daughter. “You gotta put the gun down first, honey.” Marty followed suit. “We’re here for you, OK?” he told Julia. “It’s not too late. Nothing bad has happened.”
For a moment, it seemed like Julia might relent. “OK,” she said quietly. “OK.”
Instead, she fired again.
Acting on intuition, Marty leaped at his daughter in an effort to disarm her. He wrapped his arms around her, he said, and tried to overpower her. Could it have felt to her, in that moment, like she was back in the ship scullery, trying to escape the grip of her attacker? It’s impossible to know. But she felt threatened and thrashed with all the strength she could summon, smashing at his ribs and clawing his eyes.
The gun fired again. This time, a bullet struck her mother in the thigh, tearing through a large blood vessel.
Julia didn’t realize. She fought her father for control of the gun for the next 10 minutes, pistol whipping his head until he started slipping out of consciousness. After that, she told him she loved him and went outside. He came to, and by the time she returned, had retrieved his own pistol from a drawer in the kitchen. He warned Julia he would shoot and then did, he said, striking her once in each shoulder and once in the thigh.
When the police had Julia in their custody around midnight, both she and her father were seriously injured. Her mother was dead.
The morning after the shooting, her bereaved sister Jordan called the Chico clinic, she said. She wanted someone there to explain Julia’s mental illness to the authorities, to advocate for her sister. The staff member who answered knew nothing about the shooting. “Oh shit,” Jordan recalled hearing from the other end of the phone.
That afternoon, just before 4, the clinic’s phone rang again.
It was Andrew, who was in a particularly rough place. The departure of his telepsychiatrist had made him feel cast aside yet again. He’d enrolled in an intensive VA program for people with serious mental illness, but abruptly withdrawn, believing the VA didn’t really want to help him. On the call, he asked to speak to a doctor, he recalled. When he didn’t get one, he told a pharmacist that he had not been taking his medication and was feeling paranoid again. The pharmacist encouraged him to restart the prescription and scheduled a follow-up appointment in two days.
“Vet does not appear to be a harm to himself or others,” the pharmacist wrote in Andrew’s notes.
The next day, Jan. 5, Andrew sought out the family shotgun. While Sue had gotten rid of most of the firearms in the house just a few months earlier, Andrew had kept three in his possession.
Around 12:30 p.m., Andrew called 911 and told the dispatcher he had shot his mother. He was standing in the driveway when deputies arrived.
Sue died on the scene.
Ashley first learned there had been a shooting at her mother’s house when a friend called. She initially thought Andrew had taken his own life. She and her husband raced to the house, arriving alongside first responders. Deputies wouldn’t let her on the property until well after night had fallen. Ashley struggled to make sense of what had happened. Officials told her Andrew had performed CPR on his mother. “He tried saving her life,” Ashley said.


Over the course of about 36 hours, employees’ worst fears about the Chico clinic had become reality. Many returned to the office in a state of shock.
Gradnigo, the site manager, requested a chaplain be brought into the clinic. But when she asked her supervisors what the next steps would be, she got no response, she said. Hoping the VA’s central office might intervene, she sent a tip about the shootings to the agency’s inspector general’s office, she said. She withheld her name so she wouldn’t face retaliation.
Gradnigo was fired in March 2022. The reasons provided to her were “inappropriate” comments and interactions with colleagues, records show. Gradnigo says the allegations about her conduct are exaggerated or false. She believes she lost her job because she reported wrongdoing and she is Black. She is pursuing a discrimination claim against the VA. The agency did not comment on the claim and told ProPublica it does not comment on personnel matters.
The inspector general’s office went on to investigate Julia’s case. Its report, which was published in February 2023, ticked off all the ways the clinic had failed, from medication mismanagement to not having a same-day access availability and improperly assessing her risk of violence. But the report did not mention a second patient involved in a violent act. It did not address systemic staffing issues. In fact, the office said it did not substantiate employee claims that facility leaders had failed to address their concerns about mental health staffing. The report found facility leaders had “ensured the use of telehealth and community care.”
The inspector general’s office declined to say why it did not include Andrew’s case in its report or publish a separate review. Spokesperson Fred Baker said the office reviews all complaints it receives. With respect to the employee concerns about staffing, he said, the inspector general’s office “found that leadership was taking steps to fill vacancies.”
The VA declined to make a clinic leader or official at its regional office in Sacramento available for an interview. In a statement, a Washington, D.C.-based spokesperson, Joseph Williams, said the agency “fell short” in treating Julia. “This incident does not represent the quality of care Veterans have come to expect from our facilities, or the standard to which we hold ourselves accountable, and we have taken several measures to ensure that it does not happen again,” he wrote.
The agency later said it could not answer specific questions about the care Julia or Andrew received due to privacy concerns.
After the shootings, the Chico clinic hired an on-site psychiatrist and an additional social worker, according to the inspector general report. The psychiatric nurse practitioner who prescribed the medications to Julia resigned. For the last several months, the mental health team has been fully staffed, the VA told ProPublica.
Andrew was charged with his mother’s murder in January 2022. He remains in the Butte County Jail. As early as this month, a judge could determine whether Andrew was legally sane at the time of the killing.
In an interview with ProPublica, Andrew described being stuck in a loop when he fired the shotgun. He was convinced his mom was poisoning him, something he now says was a delusion. “I love my mom,” he said. “I wish she was here.”

He doesn’t want to scapegoat the military or the VA for what happened, he said. He accepts responsibility. But he stressed that he had tried to get help from the VA repeatedly. “I do believe if there had been some form of intervention on their end, this might not have happened,” he said.
Ashley stayed in Oroville for a while, but it became impossible to go grocery shopping without someone staring at her or asking about her mother. “It felt like we were on display,” she said. Over the summer, she moved to Texas with her husband, young son and stepfather. She’s hoping to give her son the childhood she and Andrew never had.
Ashley is still mourning her mother, whom she described as a devoted grandmother and her closest friend. She has also been doing whatever she can to support Andrew in jail. She calls and texts him regularly and makes sure he has enough money in his account for the commissary. When he texted about playing Dungeons & Dragons recently, she replied like a mother might. “I’m so happy that you’re doing something fun,” she wrote. “I love you, Andrew.”


Julia was also charged criminally for her mother’s death. In January 2023, she was found not guilty by reason of insanity. She is now a patient at Patton State Hospital, a sprawling forensic psychiatric complex at the base of the San Bernardino Mountains about 60 miles east of Los Angeles. She reads books in the library, helps organize group activities like bingo and keeps her fingernails painted vibrant colors. She has a journal with positive affirmations on each page; she writes down the things she’s grateful for.
For some time after the shooting, Julia didn’t know she had caused her mother’s death. It was only after listening to the 911 recording months later that she began to understand what had happened. Coming to grips with that has been excruciating, she said. Her mom was her best friend. On a recent afternoon, during an open mic event at the hospital, she read a poem she wrote about their relationship. Audience members were brought to tears, she said.
It is hard to say what prompted the shooting. She recalls hearing an explosion in the distance — maybe a gas tank — and feeling like she needed to protect herself from some unknown threat. “It felt like I was unconscious, not awake,” she told a psychologist who evaluated her in January 2023, records show. “It felt like I was in a video game.” The psychologist speculated the explosion triggered her PTSD and may have put her in a dissociated state.
Julia isn’t sure how long she’ll be at Patton. She would have to be cleared by the hospital and the court to be released for supervised treatment in the community.


It has taken many months for Marty to begin recovering. His ribs were fractured and his back was broken in two places. He needed 15 staples in his head. The emotional recovery, he knows, will be much longer. He’s chosen to stay in the hilltop ranch where the shooting took place. He bought the property to grow old there, and that’s what he still intends to do. He finds comfort in his fruit trees and livestock and the sweeping mountain views.
He said he forgives his daughter. He keeps her military photo in his wallet. But he is furious at the VA. “I want to punch VA in the face,” he said one afternoon late in the summer, while the sun poured into his den. To him, it was obvious what had needed to happen and what went wrong.
It crystallized deep in his mind the night of the shooting, after Julia had finally relented and he picked up Candy’s cellphone to speak with the 911 operator.
“She really, really needs help,” he told the operator while waiting for the police to come and arrest his daughter. “We tried to get her help at the VA. And, God, the VA didn’t really help that much.”
The dispatcher was empathetic. She’d heard Julia’s cries for help all night; dozens of them were captured in a recording of the call.
“I’m sorry the VA didn’t help her,” the dispatcher said.
Editor’s Note
After reading a February 2023 report by the Department of Veterans Affairs’ Office of Inspector General about inadequate mental health care at a VA clinic in Chico, California — a document that did not name any veterans or health care professionals or provide specific dates — ProPublica reporters wanted to more fully understand the tragedy that unfolded and what lessons it offered for the larger VA health care system. They spent months investigating the case at the center of the report involving a veteran named Julia Larsen as well as a second case involving a veteran named Andrew Iles who was also treated at the clinic.
The reporters interviewed Julia in person at Patton State Hospital near San Bernardino, California, and spent many hours interviewing her by telephone and video call. They traveled to St. Louis to meet with her attorneys. They reviewed hundreds of pages of her military personnel and medical records, as well as police reports from the night of the shooting and transcripts of interviews Julia gave to detectives and psychologists after her arrest. They listened to the 911 call Julia’s mother, Candy Larsen, made before she died. They interviewed Julia’s father, Marty Larsen, at his home in Red Bluff, California. They interviewed her sister Jordan Pepper, childhood friend Brittney Apel and former boyfriend Ignacio Gutierrez by telephone. In addition to Brittney and Ignacio, who served in the Navy with Julia, they interviewed four other people who knew Julia from the military, one of whom Julia told about the sexual assault and corroborated her recollections. They also interviewed Laurie Smith, a close friend of Julia’s mother.
The reporters interviewed Andrew in person at the Butte County Jail in Oroville, California, and by telephone. They reviewed some of his medical records, military performance reviews and discharge records, as well as his court records and family photos from his childhood. They interviewed his sister, Ashley Hill, at her home in Texas and his half-brother William Iles, aunt MaryJo Hendricks, former girlfriend Kayley Reni and childhood friend Alex Kenworthy by telephone. They interviewed a second childhood friend who declined to be named.
Both Julia and Andrew consented to ProPublica publishing information from their medical records about their diagnoses and medical histories.
To better understand the issues at the Chico clinic, the reporters interviewed a half-dozen current and former employees. They reviewed emails sent between 2016 and 2022 that detailed staffing issues, as well as hundreds of pages in former site manager Michelle Gradnigo’s discrimination complaint. They also reviewed an internal proposal from 2021 to grow the virtual mental health program and documents from the Office of Inspector General’s investigation obtained through Freedom of Information Act requests.
To put the case into broader context, the reporters reviewed and analyzed more than 300 routine inspections and investigative reports published by the VA’s inspector general since January 2020, some examining events that occurred in 2019. They brought their findings to experts and interviewed the relatives of three veterans who died by suicide after receiving inadequate mental health care from the VA. They reviewed national reports on mental health staffing and outcomes.
Overall, the reporters spoke to more than a dozen mental health professionals, researchers and policy experts. They consulted with some on how to interview people who have experienced trauma and been diagnosed with severe mental illness. They asked others to describe how the treatment Julia and Andrew received from the Chico VA clinic differed from generally established standards of care and offer insight into the issues facing the VA’s health system.